A Practical Guide to ICH Q2(R1) Method Validation for Pharmaceutical Residue Analysis
This article provides a comprehensive guide for researchers and drug development professionals on applying ICH Q2(R1) guidelines to the validation of analytical methods for pharmaceutical residue analysis. It covers foundational principles, from understanding regulatory requirements and defining key validation parameters like specificity, accuracy, and precision, to their practical application in methods for cleaning validation and impurity testing. The content further addresses common troubleshooting scenarios, optimization strategies for low-level residue detection, and the implementation of modern, risk-based lifecycle approaches, including trends toward ICH Q2(R2) and Quality-by-Design (QbD). The goal is to equip scientists with the knowledge to develop robust, compliant, and reliable analytical procedures that ensure product safety and quality.
A Practical Guide to ICH Q2(R1) Method Validation for Pharmaceutical Residue Analysis
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on applying ICH Q2(R1) guidelines to the validation of analytical methods for pharmaceutical residue analysis. It covers foundational principles, from understanding regulatory requirements and defining key validation parameters like specificity, accuracy, and precision, to their practical application in methods for cleaning validation and impurity testing. The content further addresses common troubleshooting scenarios, optimization strategies for low-level residue detection, and the implementation of modern, risk-based lifecycle approaches, including trends toward ICH Q2(R2) and Quality-by-Design (QbD). The goal is to equip scientists with the knowledge to develop robust, compliant, and reliable analytical procedures that ensure product safety and quality.
Understanding ICH Q2(R1) and Its Role in Pharmaceutical Residue Control
The Critical Importance of Validated Methods for Residue and Impurity Analysis
In the development and manufacturing of biopharmaceuticals, profiling process-related impurities and residuals is not merely a scientific best practice but a firm regulatory expectation [1] [2]. These impurities, which can be introduced at various stages of bioprocessing—from upstream cell culture to downstream purification—must be monitored and controlled to ensure patient safety and product quality [1] [3]. Because these residuals are typically present at low levels within complex and variable sample matrices, the development, validation, and application of robust analytical methods present a significant scientific challenge [1] [2]. The International Council for Harmonisation (ICH) Q2(R1) guideline, "Validation of Analytical Procedures," provides the foundational framework for demonstrating that an analytical method is fit for its intended purpose, ensuring the reliability, accuracy, and consistency of the data used to make critical decisions about drug substance and drug product quality [4] [5].
Adherence to ICH Q2(R1) is crucial for global regulatory submissions, and it outlines the key validation parameters required for a variety of analytical procedures [4] [6]. This article will explore the major classes of process-related impurities, compare the analytical techniques used for their detection, and detail the experimental protocols for method validation, all within the critical context of ICH Q2(R1).
Bioprocessing is a complex sequence of steps, each of which can introduce specific residual impurities that must be cleared from the final product [1] [2]. These impurities can be broadly categorized based on their origin in the manufacturing process.
Table 1: Common Classes of Process-Related Impurities
| Impurity Class | Examples | Typical Origin in Process |
|---|---|---|
| Host Cell-Derived | Host Cell Proteins (HCP), DNA, RNA [1] [2] | Cell lysis following upstream culture [1] |
| Upstream Additives | Antibiotics (e.g., Kanamycin, Gentamicin), Inducers (e.g., IPTG) [1] [2] | Cell-culture media to control contamination or induce expression [1] |
| Process-Enhancing Agents | Solubilizers (e.g., Guanidine, Urea), Reducing Agents (e.g., DTT, Glutathione) [1] [2] | Steps for solubilization, reduction, and refolding of proteins [1] |
| Downstream Reagents | Surfactants (e.g., Triton X-100, Tween), Chromatographic Ligands, Organic Solvents [1] [2] [3] | Purification, separation, and formulation steps [1] |
| Extractables & Leachables | Phthalates, Antioxidants, Metal Ions [2] [3] | Single-use bioprocessing systems like bags, filters, and tubing [2] |
Analytical Techniques for Impurity Monitoring
A diverse array of analytical techniques is required to detect and quantify the wide range of potential residual impurities, each with specific strengths for different types of analytes and matrices.
Table 2: Comparison of Key Analytical Techniques for Residual Impurity Analysis
| Analytical Technique | Best Suited For | Typical Sensitivity | Key Advantages |
|---|---|---|---|
| LC-MS/MS (Liquid Chromatography with Tandem Mass Spectrometry) | Non-volatile organics (Antibiotics, Surfactants, Inducers) [1] [3] | Part-per-billion (ppb) levels [1] [2] | High selectivity and sensitivity; uses specific daughter ions for quantification [1] |
| GC-MS (Gas Chromatography-Mass Spectrometry) | Volatile and semi-volatile organics (Residual Solvents) [1] [2] | Varies by analyte and detector | Robust technique for volatile impurities; can use headspace sampling [1] |
| ICP-MS (Inductively Coupled Plasma-Mass Spectrometry) | Elemental Impurities (Metal Ions, Inorganics) [2] [3] | Very high (e.g., parts-per-trillion) | Capable of multi-element analysis; extremely sensitive for metals [3] |
| Ion Chromatography (IC) | Ionic species [1] | Low concentrations of ions [1] | High selectivity for charged molecules [1] |
| PCR (Polymerase Chain Reaction) | Residual Host Cell DNA [1] [2] | High (amplifies few copies) [1] | Highly specific and sensitive for trace DNA contamination [1] |
| ELISA (Enzyme-Linked Immunosorbent Assay) | Host Cell Proteins (HCP) [1] [2] | Varies by kit | High throughput; specific to a given cell line [1] |
Experimental Protocols for Key Techniques
Protocol 1: LC-MS/MS for Trace Antibiotic Analysis
- Sample Preparation: The complex sample matrix, often containing the protein of interest, may require protein precipitation. The supernatant is obtained via centrifugation or filtration, with validation to ensure the target impurity is not co-precipitated [1]. Further sample clean-up may involve liquid-liquid extraction [1].
- Chromatographic Separation: The sample is introduced to a High Performance Liquid Chromatography (HPLC) system, where components of the mixture are separated based on their partition between a stationary phase and a mobile phase gradient [2].
- Detection & Quantification: Eluting components are ionized in the mass spectrometer's ion source (e.g., by electrospray). The triple quadrupole mass analyzer first selects the parent ion of the target antibiotic, fragments it in a collision cell, and then selects a specific daughter ion for highly selective and sensitive quantification, often using Multiple Reaction Monitoring (MRM) [2] [3]. The use of internal standards is common for accurate quantitation [2].
Protocol 2: PCR for Residual DNA Clearance
- DNA Extraction: Genomic DNA is isolated from the sample.
- Amplification: The DNA is heat-denatured into single strands. Specific oligonucleotide primers complementary to the 3' ends of the target host cell DNA sequence are added in excess. These primers hybridize with their complementary sequences when the temperature is lowered. A heat-stable DNA polymerase (e.g., Taq polymerase) then extends the primers to synthesize new DNA strands [2].
- Detection: The cycle of denaturation, annealing, and extension is repeated multiple times, exponentially amplifying the target DNA fragment to a detectable level, confirming the presence and allowing for quantification of residual DNA [1] [2].
The ICH Q2(R1) Validation Framework
The ICH Q2(R1) guideline, "Validation of Analytical Procedures," provides a harmonized framework for validating analytical methods to ensure they are reliable and reproducible for their intended use [4] [5]. It defines the key validation characteristics that must be evaluated.
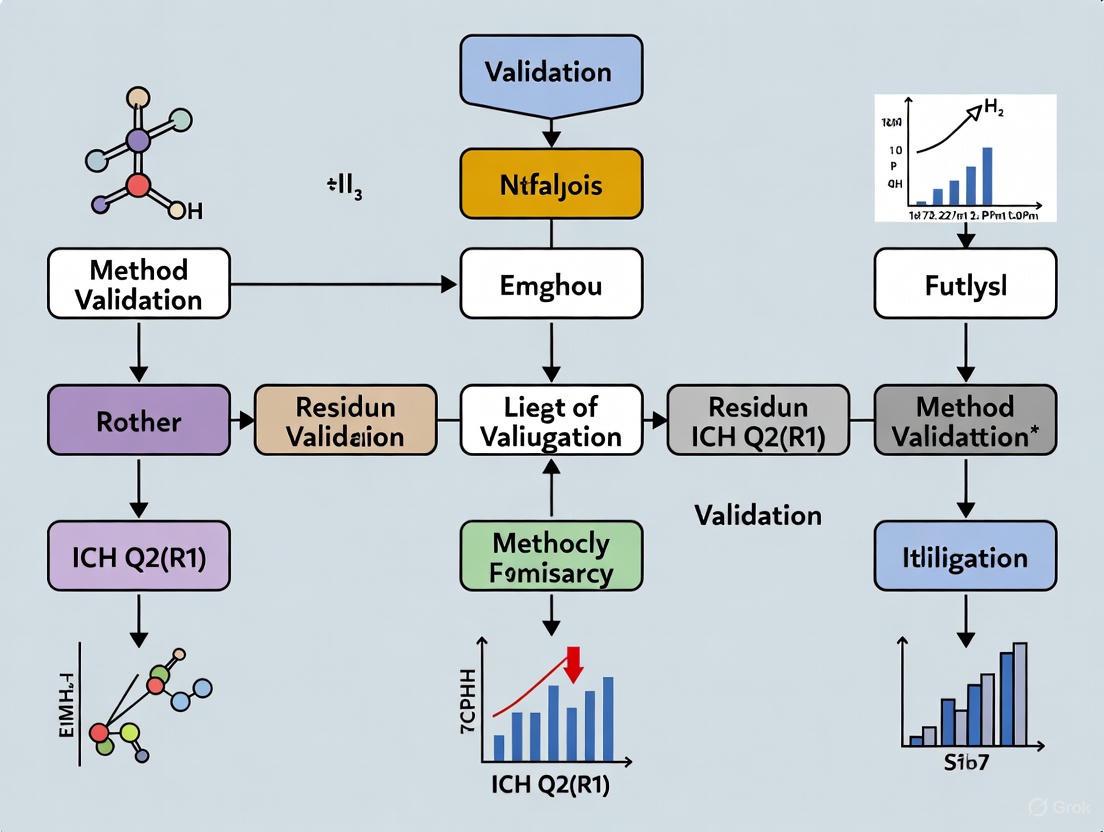
Diagram 1: ICH Q2(R1) Method Validation Workflow. This flowchart illustrates the interconnected sequence of validation parameters that must be assessed to confirm an analytical procedure is fit for purpose.
Table 3: Core Validation Parameters as Defined by ICH Q2(R1)
| Validation Parameter | Definition | Experimental Approach for Impurity Methods |
|---|---|---|
| Specificity | Ability to assess the analyte unequivocally in the presence of other components [5] | Demonstrate resolution of impurity peak from the main product and other potential impurities (e.g., degradants) [5] |
| Accuracy | Closeness of test results to the true value [5] | Spike recovery experiments in the sample matrix (e.g., drug substance/product) at known concentrations [5] |
| Precision | Degree of agreement among individual test results (includes repeatability and intermediate precision) [5] | Multiple analyses of homogeneous sample by same analyst (repeatability) and different analysts/days/instruments (intermediate precision) [5] |
| Linearity | Ability to obtain results proportional to analyte concentration [5] | Analyze samples with impurity across a defined range (e.g., from LOQ to 120% or 150% of specification) [5] |
| Range | Interval between upper and lower concentration with suitable linearity, accuracy, and precision [5] | Established based on linearity data and the intended use of the method (e.g., from LOQ to 150% of specification) [5] |
| LOD / LOQ | Lowest amount detected (LOD) or quantified with accuracy and precision (LOQ) [5] | Signal-to-noise ratio or based on the standard deviation of the response and the slope of the calibration curve [5] |
| Robustness | Capacity to remain unaffected by small, deliberate variations in method parameters [5] | deliberate variations in parameters (e.g., HPLC column temperature, mobile phase pH, flow rate) [5] |
The Scientist's Toolkit: Essential Reagents and Materials
The development and execution of validated methods for residue analysis require specific, high-quality reagents and materials.
Table 4: Key Research Reagent Solutions for Impurity Analysis
| Reagent / Material | Function in Analysis |
|---|---|
| Stable Isotope-Labeled Internal Standards | Added to the sample prior to analysis by LC-MS/MS or GC-MS to correct for matrix effects and losses during sample preparation, improving accuracy and precision [2]. |
| Certified Reference Standards | Highly purified and well-characterized analytes used for calibration and qualification; essential for demonstrating method accuracy and linearity [5]. |
| MS-Grade Mobile Phase Modifiers | High-purity solvents and additives (e.g., formic acid, ammonium acetate) for LC-MS that minimize background noise and ion suppression, enhancing sensitivity [1]. |
| Specific Antibodies for ELISA | Antibodies raised against a spectrum of Host Cell Proteins (HCP) from the specific production cell line; critical for the specificity of HCP assays [1] [2]. |
| Sequence-Specific Primers for PCR | Synthetic oligonucleotides designed to be complementary to the host cell's genomic DNA; ensure the specific and sensitive amplification of residual DNA [2]. |
Within the highly regulated biopharmaceutical industry, the critical importance of validated methods for residue and impurity analysis is unequivocal. The ICH Q2(R1) guideline provides the essential, globally recognized framework for proving that these analytical procedures are scientifically sound and fit for their purpose—ensuring that potentially harmful process residuals are accurately monitored and controlled to safe levels [4] [5]. As the industry evolves with more complex molecules and advanced technologies, the principles of ICH Q2(R1) remain the bedrock of quality control. The strategic application of sophisticated techniques like LC-MS/MS and PCR, guided by a thorough understanding of validation parameters, is fundamental to upholding the highest standards of patient safety and drug product quality.
Defining the Four Core Types of Analytical Procedures in ICH Q2(R1)
Analytical procedures are fundamental to ensuring the identity, purity, and content of pharmaceutical products, forming the foundation of product quality and patient safety [7]. The International Council for Harmonisation (ICH) Q2(R1) guideline, titled "Validation of Analytical Procedures: Text and Methodology," serves as the globally recognized standard for validating these analytical methods [8] [9]. This guideline harmonizes requirements across major regulatory regions, including the United States, Europe, and Japan, providing a unified framework for pharmaceutical analysis [9]. Validation under ICH Q2(R1) demonstrates that an analytical procedure is suitable for its intended purpose and will yield reliable and reproducible results throughout its lifecycle [7]. For researchers focused on pharmaceutical residue analysis, a thorough understanding of these procedure categories and their respective validation requirements is not just a regulatory formality but a critical scientific endeavor to ensure data integrity and product quality.
The Four Core Types of Analytical Procedures
The ICH Q2(R1) guideline primarily categorizes analytical procedures based on their fundamental objectives in assessing pharmaceutical quality. These categories directly address the core quality attributes of a drug substance or product.
Identification Tests
Purpose and Scope: Identification tests are designed to confirm the identity of an analyte in a given sample, ensuring that the drug substance present is indeed what is declared [7]. This is a fundamental requirement for all pharmaceutical products, as it verifies that the patient is receiving the correct active pharmaceutical ingredient. These tests typically work by comparing a property of the sample analyte to that of a authenticated reference standard.
Common Techniques and Examples:
- Spectroscopic Techniques: Techniques such as Infrared (IR) spectroscopy or Mass Spectrometry (MS) are commonly used for identity confirmation by matching spectral fingerprints to reference materials [10].
- Immunoassays: Techniques like Western Blotting or immunofluorescence use specific antibody-antigen interactions to identify proteins or viral antigens, commonly applied for biologics and vaccines [7].
- Genetic Methods: Polymerase Chain Reaction (PCR) is employed for identifying viral vaccines or products containing nucleic acids by amplifying specific, unique gene sequences [7].
- Chromatographic Methods: High-Performance Liquid Chromatography (HPLC) with retention time matching against a reference standard can serve as an identity test.
- Simple Chemical Tests: Pharmacopoeias often include straightforward identification methods such as color reactions or precipitation tests for active pharmaceutical ingredients [7].
Testing for Impurities
Purpose and Scope: Impurity tests are crucial for defining the purity profile of a drug substance or product, detecting and quantifying unwanted chemical species that may arise from synthesis, degradation, or storage [7]. These procedures ensure that all impurities are below acceptable safety thresholds, thereby demonstrating the product's harmlessness to patients. Impurity testing can be performed as either quantitative tests, which determine the exact amount of an impurity present, or limit tests, which simply verify that an impurity is below a specified acceptance level [7].
Common Techniques and Examples:
- Chromatographic Methods: HPLC with various detectors (UV, MS) is the workhorse for impurity separation and quantification, especially for related substances in small molecules.
- Limit Tests for Contaminants: Tests for residual solvents, heavy metals, or arsenic often employ specific limit tests as described in pharmacopoeias [7].
- Electrophoretic Techniques: Capillary Electrophoresis (CE) is used for separating charged impurities, particularly relevant for biologics like proteins and peptides.
Assays (Content/Potency)
Purpose and Scope: Assays are quantitative procedures designed to measure the amount or potency of the major analyte in a sample [7]. These tests serve two primary functions: they determine the content of the active pharmaceutical ingredient (how much is present) and they may assess the potency (biological activity) of the substance. This dual approach ensures that the drug contains the claimed amount of active ingredient and that the ingredient possesses the intended therapeutic activity.
Common Techniques and Examples:
- Content Assays: UV-Vis spectrophotometry for concentration determination or HPLC-UV assays for specific compound quantification are standard for content determination [7].
- Potency Assays (Bioassays): For biologics, cell-based assays measure the biological effect of a molecule, such as a clot lysis assay for tissue plasminogen activator (tPA) or cell proliferation assays for growth factors [7].
- Viral Titrations: For live viral vaccines, Plaque Forming Unit (PFU) assays determine the concentration of infectious virus particles, which correlates with vaccine potency [7].
- Enzymatic Activity Assays: These measure the catalytic activity of enzyme therapeutics, often using substrate-to-product conversion metrics.
Table 1: Core Analytical Procedure Types in ICH Q2(R1)
| Procedure Type | Primary Objective | Key Validation Parameters | Common Examples |
|---|---|---|---|
| Identification Tests | To verify the identity of an analyte [7] | Specificity [7] | IR spectroscopy, PCR, peptide mapping [7] |
| Impurity Tests (Quantitative) | To accurately measure impurity content [7] | Specificity, Accuracy, Precision, LOD, LOQ, Linearity, Range [7] | HPLC-UV/MS for related substances [7] |
| Impurity Tests (Limit Tests) | To ensure impurities are below a specified limit [7] | Specificity, LOD [7] | Heavy metals testing, residual solvents [7] |
| Assays | To quantify the major analyte or its potency [7] | Specificity, Accuracy, Precision, Linearity, Range [7] | HPLC assay for content, cell-based bioassays [7] |
Method Validation Parameters Across Procedure Types
The validation parameters required for each analytical procedure type vary according to its intended use and criticality. ICH Q2(R1) defines a set of characteristic parameters that must be validated to demonstrate procedure suitability.
Definition of Validation Parameters
- Specificity: The ability to assess unequivocally the analyte in the presence of components that may be expected to be present, such as impurities, degradation products, or matrix components [7] [9]. For identification tests, this is the critical parameter [7].
- Accuracy: The closeness of agreement between the value found and the value accepted as a true or reference value. It expresses the trueness of the method [9].
- Precision: The closeness of agreement between a series of measurements from multiple sampling of the same homogeneous sample under prescribed conditions. It includes repeatability, intermediate precision, and reproducibility [9].
- Linearity: The ability of the method to obtain test results directly proportional to the concentration of the analyte within a given range [9].
- Range: The interval between the upper and lower levels of analyte that have been demonstrated to be determined with suitable levels of precision, accuracy, and linearity [9].
- Detection Limit (DL): The lowest amount of analyte in a sample that can be detected, but not necessarily quantified [9].
- Quantitation Limit (QL): The lowest amount of analyte in a sample that can be quantitatively determined with suitable precision and accuracy [9].
- Robustness: A measure of the procedure's capacity to remain unaffected by small, deliberate variations in method parameters, indicating its reliability during normal usage [9].
Parameter Requirements by Procedure Type
Table 2: Validation Parameter Requirements by Analytical Procedure Type
| Validation Parameter | Identification | Impurity Tests (Quantitative) | Impurity Tests (Limit) | Assays |
|---|---|---|---|---|
| Specificity | Yes [7] | Yes [7] | Yes [7] | Yes [7] |
| Accuracy | No | Yes [7] | No | Yes [7] |
| Precision | No | Yes [7] | No | Yes [7] |
| Linearity | No | Yes [7] | No | Yes [7] |
| Range | No | Yes [7] | No | Yes [7] |
| Detection Limit (DL) | No | No | Yes [7] | No |
| Quantitation Limit (QL) | No | Yes [7] | No | No |
Analytical Procedure Workflow and Lifecycle
The following diagram illustrates the logical workflow for selecting, developing, and validating an analytical procedure based on the ICH Q2(R1) framework and its subsequent evolution toward a full lifecycle approach.
Essential Research Reagent Solutions for Analytical Procedures
The successful implementation of analytical procedures according to ICH Q2(R1) requires carefully selected reagents and materials to ensure reliability and reproducibility.
Table 3: Essential Research Reagents and Materials for Analytical Method Validation
| Reagent/Material | Function/Purpose | Application Examples |
|---|---|---|
| Reference Standards | Provides an authentic sample of the analyte with known identity and purity for comparison and calibration [7]. | Identification tests, assay calibration, impurity quantification [7]. |
| Critical Reagents | Specific binding reagents essential for the function of certain bioanalytical methods. | Antibodies for immunoassays, enzymes for enzymatic activity tests, cell lines for bioassays [7]. |
| Chromatographic Materials | Stationary phases and columns for separation sciences. | HPLC/UPLC columns for impurity profiling, assay content determination. |
| Sample Preparation Reagents | Solvents, extraction buffers, dilution media, and derivatization agents. | Protein precipitation solvents, solid-phase extraction cartridges, dilution buffers for sample preparation. |
| System Suitability Solutions | Mixtures used to verify that the analytical system is operating correctly before sample analysis. | Resolution mixtures for chromatography, precision standards for injection repeatability. |
Regulatory Context and Evolution to ICH Q2(R2)
While ICH Q2(R1) remains the current implemented guideline in most regions, understanding its evolution provides valuable context for pharmaceutical analysts. The ICH has recently finalized Q2(R2) on "Validation of Analytical Procedures" and introduced Q14 on "Analytical Procedure Development" [11]. These updates reflect the increasing complexity of pharmaceutical products, particularly biologics, and the advancement of analytical technologies.
Key enhancements in Q2(R2) include:
- Formalization of a lifecycle approach to analytical procedures, advocating for continuous validation and assessment throughout the method's operational use [11].
- Enhanced method development principles incorporating Quality by Design (QbD) and defining an Analytical Target Profile (ATP) early in development [11] [12].
- Refinements to validation parameters, including explicit guidance for multivariate methods and non-linear responses [11] [10].
- Mandatory robustness testing integrated with the lifecycle approach [11].
For researchers conducting pharmaceutical residue analysis, these developments emphasize the importance of robust, well-developed methods from the outset, with validation parameters carefully selected based on the specific analytical question being addressed—whether it concerns identity, purity, or content.
The validation of analytical methods is a critical prerequisite in pharmaceutical research to ensure that the data generated is reliable and fit for its intended purpose. For residue analysis, which often involves quantifying trace levels of substances, demonstrating that a method is rigorously characterized is paramount. The International Council for Harmonisation (ICH) Q2(R1) guideline provides a foundational framework for this process, outlining the key parameters that must be evaluated. This guide focuses on four of these essential parameters—Specificity, Limit of Detection (LOD), Limit of Quantitation (LOQ), and Accuracy—by comparing different analytical approaches, detailing experimental protocols, and presenting objective performance data to inform method development and validation.
Specificity: Ensuring Analytical Selectivity
Specificity is the ability of an analytical method to unequivocally assess the analyte in the presence of other components that may be expected to be present, such as impurities, degradation products, or matrix components [13]. A specific method ensures that the signal measured is solely due to the target analyte.
Experimental Protocol for Demonstrating Specificity
To challenge the specificity of a method, a series of experiments should be performed [13]:
- Analyze a blank sample: The sample matrix (e.g., plasma, tissue homogenate) without the analyte should be analyzed to demonstrate the absence of interfering signals at the retention time of the analyte.
- Analyze a spiked sample: The sample matrix spiked with the analyte at a relevant concentration (e.g., the LOQ) should be analyzed to confirm the analyte's response.
- Challenge with potential interferents: The sample matrix should be spiked with the analyte and all potential interferents. These typically include:
- Degradation products (from forced degradation studies)
- Process impurities
- Excipients (for drug products)
- Other analytes that may be co-administered or co-extracted.
- Chromatographic examination: For chromatographic methods like HPLC, the resulting chromatograms are examined for baseline resolution. The method is considered specific if the analyte peak is unaffected by the presence of interferents and no significant interference is observed at the same retention time.
Limits of Detection (LOD) and Quantitation (LOQ): Defining Method Sensitivity
The Limit of Detection (LOD) is the lowest amount of analyte that can be detected, but not necessarily quantified, under the stated experimental conditions. The Limit of Quantitation (LOQ) is the lowest amount of analyte that can be quantitatively determined with acceptable precision and accuracy [14] [13]. These parameters are crucial for residue methods where analytes are present at very low concentrations.
Comparison of Calculation Approaches
There is no universal protocol for determining LOD and LOQ, and different approaches can yield significantly different results [15] [16]. The ICH Q2(R1) guideline describes several methods, each with its own advantages and applications [13] [17].
Table 1: Comparison of Common Approaches for Determining LOD and LOQ
| Approach | Description | Typical Formula | Advantages | Disadvantages |
|---|---|---|---|---|
| Signal-to-Noise (S/N) [18] [19] | Measures the ratio of the analyte signal to the background noise. | LOD: S/N ≥ 2 or 3LOQ: S/N ≥ 10 | Simple, intuitive, and directly applicable to chromatographic methods. | Can be subjective; depends on how noise is measured; may not account for matrix effects. |
| Standard Deviation of the Blank [14] [19] | Based on the mean and standard deviation (SD) of the response from multiple blank samples. | LOB = Meanblank + 1.645*SDblankLOD = LOB + 1.645*SD_low concentration sample | Statistically rigorous; defined in CLSI EP17 guideline. | Requires a large number of replicates; a genuine analyte-free blank matrix can be difficult to obtain. |
| Calibration Curve: SD of Response & Slope [13] [17] | Uses the standard error of the regression (or y-intercept) and the slope of the calibration curve. | LOD = 3.3σ / SLOQ = 10σ / SWhere σ = standard deviation of response, S = slope | Scientifically robust; uses data from the calibration curve; does not require a separate blank. | Assumes the calibration curve is linear in the low-concentration range; the estimate of σ can vary. |
| Accuracy Profile [15] [18] | A graphical tool based on tolerance intervals that combines bias and precision to define the lowest level meeting accuracy criteria. | Based on β-content tolerance intervals | Provides a realistic and relevant assessment; considers total error. | More complex to compute and implement. |
| Visual Evaluation [13] [19] | The lowest concentration is determined by the analyst or instrument to be reliably detected or quantified. | Determined by logistic regression of binary (detect/non-detect) data. | Practical for non-instrumental methods (e.g., visual tests). | Subjective and highly variable between analysts. |
Experimental Data and Protocol for Calibration Curve Method
A practical example for calculating LOD and LOQ via the calibration curve method using HPLC is provided below [17].
- Procedure:
- Prepare a calibration curve with at least 5 concentrations in the range of the expected LOD/LOQ.
- Inject each calibration level and record the analyte response (e.g., peak area).
- Perform a linear regression analysis on the data (Concentration vs. Response) to obtain the slope (S) and the standard error of the regression (σ, or ( s_{y/x} )).
- Sample Calculation:
- From the regression output: Slope (S) = 1.9303, Standard Error (σ) = 0.4328.
- LOD = (3.3 × 0.4328) / 1.9303 = 0.74 ng/mL
- LOQ = (10 × 0.4328) / 1.9303 = 2.24 ng/mL [17]
- Validation: The calculated LOD and LOQ must be verified experimentally by preparing and analyzing multiple replicates (e.g., n=6) at these concentrations. The LOQ, in particular, should demonstrate an accuracy and precision (e.g., %CV) within ±20% [18].
Table 2: Comparison of LOD/LOQ Values for Different Drugs Using Various Methods [16]
| Analyte | Calculation Method | LOD | LOQ |
|---|---|---|---|
| Carbamazepine | Signal-to-Noise (S/N) | Lowest Value | Lowest Value |
| Carbamazepine | Standard Deviation of Response (SDR) | Highest Value | Highest Value |
| Phenytoin | Signal-to-Noise (S/N) | Lowest Value | Lowest Value |
| Phenytoin | Standard Deviation of Response (SDR) | Highest Value | Highest Value |
This table highlights that the choice of calculation method significantly influences the reported sensitivity of a method, underscoring the need to specify the approach used.
Figure 1: A generalized workflow for determining and validating the Limit of Detection (LOD) and Limit of Quantitation (LOQ), incorporating common calculation methods and the essential step of experimental confirmation.
Accuracy: Establishing Trueness of Measurement
Accuracy expresses the closeness of agreement between the value found and the value accepted as a true or reference value. It is often reported as percent recovery of the known, spiked amount of analyte [13]. For residue methods, accuracy is typically assessed across the validated range, including the LOQ.
Experimental Protocol for Assessing Accuracy
The following protocol is standard for evaluating accuracy in bioanalytical methods:
- Sample Preparation: Prepare a minimum of five replicates per concentration level. Accuracy should be evaluated at a minimum of three concentration levels (low, medium, and high) within the range of the method [13].
- Spiking: Spike the analyte of interest into the blank matrix (e.g., plasma) at the known concentrations.
- Analysis: Analyze the spiked samples using the validated method.
- Calculation: Calculate the mean measured concentration for each level and determine the accuracy as % Recovery:
- % Recovery = (Mean Measured Concentration / Nominal Spiked Concentration) × 100
- Acceptance Criteria: For bioanalytical methods, accuracy should be within ±15% of the nominal value, except at the LOQ, where it should be within ±20% [18].
Table 3: Example Accuracy and Precision Data for a Residue Method
| Nominal Concentration (ng/mL) | Mean Measured Concentration (ng/mL) | Accuracy (% Recovery) | Precision (%CV) |
|---|---|---|---|
| 2.5 (LOQ) | 2.45 | 98.0% | 5.2% |
| 50.0 | 51.2 | 102.4% | 3.1% |
| 100.0 | 97.8 | 97.8% | 2.0% |
The Scientist's Toolkit: Essential Reagents and Materials
The following table lists key materials required for the development and validation of residue methods, particularly those based on HPLC.
Table 4: Essential Research Reagent Solutions and Materials
| Item | Function / Purpose |
|---|---|
| Blank Matrix | The analyte-free biological material (e.g., plasma, urine, tissue homogenate) used to prepare calibration standards and quality control samples. It is critical for assessing specificity and matrix effects [20]. |
| Reference Standard | A highly characterized substance of known purity and identity used to prepare the analyte stock and working solutions for spiking [13]. |
| Internal Standard (IS) | A compound added in a constant amount to all samples, blanks, and calibration standards to correct for variability during sample preparation and instrument analysis [15]. |
| Mobile Phase Solvents | High-purity solvents (e.g., HPLC-grade methanol, acetonitrile, water) and buffers used to elute the analyte from the chromatographic column. |
| Sample Preparation Materials | Supplies for extraction and purification, such as solid-phase extraction (SPE) cartridges, protein precipitation plates, and liquid-liquid extraction solvents. |
The validation of specificity, LOD, LOQ, and accuracy forms the cornerstone of a reliable analytical method for pharmaceutical residue analysis. As demonstrated, multiple approaches exist for determining LOD and LOQ, each with its own merits and limitations. The classical statistical methods can sometimes provide underestimated values, while more modern graphical tools like the accuracy or uncertainty profile offer a more realistic assessment by incorporating total error [15]. The choice of method should be justified and aligned with the regulatory guidelines and the intended use of the method. Ultimately, whichever parameters and calculation methods are selected, they must be supported by robust experimental data and rigorous validation protocols to ensure the method is truly fit for purpose.
For researchers and scientists in drug development, navigating the regulatory requirements of major health authorities is a critical component of bringing pharmaceutical products to market. The International Council for Harmonisation (ICH) provides a foundational framework through guidelines like ICH Q2(R1) on analytical method validation, which establishes harmonized standards for validating analytical procedures. These guidelines form the scientific and regulatory bedrock for ensuring that analytical methods used in pharmaceutical residue analysis are reliable, reproducible, and fit for their intended purpose [5].
While ICH guidelines create a platform for harmonization, regulatory authorities in different regions implement and enforce these standards with varying emphases and additional requirements. The U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) represent two of the most influential regulatory bodies whose compliance standards impact global drug development. Understanding their distinct approaches, particularly in areas such as Current Good Manufacturing Practices (CGMP), inspection procedures, and the management of post-approval changes, is essential for successful regulatory strategy and global market access [21] [22].
This guide provides a comparative analysis of the regulatory landscapes of the FDA and EMA, with a specific focus on requirements relevant to pharmaceutical residue analysis research. It is structured within the context of method validation according to ICH Q2(R1) guidelines, providing scientists with practical frameworks for compliance and operational excellence.
Comparative Analysis of FDA and EMA Regulatory Requirements
The following table summarizes the key regulatory aspects of the FDA and EMA relevant to pharmaceutical analysis and method validation.
Table 1: Key Regulatory Requirements Comparison for Pharmaceutical Analysis
| Aspect | U.S. FDA (Food and Drug Administration) | EMA (European Medicines Agency) |
|---|---|---|
| Primary Legal Framework | Federal Food, Drug, and Cosmetic Act; 21 CFR Parts 210 & 211 (CGMP) [21] | Directive 2001/83/EC; Regulation (EC) No 726/2004 [22] |
| GMP/GDP Regulations | Current Good Manufacturing Practice (CGMP) in 21 CFR 210, 211, and 212 [21] | EU GMP Guidelines; EudraGMDP database for certificates and non-compliance statements [22] |
| Guidance on Method Validation | Adheres to ICH Q2(R1) and Q2(R2); FDA guidance documents [5] | Adheres to ICH Q2(R1) and Q2(R2); EU GMP Annexes [22] |
| Approach to Inspections | Risk-based pre-approval and surveillance inspections; Domestic and international inspections [23] | Risk-based inspections by National Competent Authorities; Mutual Recognition Agreements (MRAs) for non-EU sites [22] |
| Lifecycle Management | CFR 314.70 for post-approval changes; Emerging advanced manufacturing guidance (2025) [24] | EU Variations Guidelines (2025) with Types IA, IB, and II; PACMPs and PLCM documents [25] |
| Governance of Analytical Procedures | ICH Q2(R2) and Q14 on Analytical Procedure Lifecycle [5] | ICH Q2(R2) and Q14; Compilation of Union procedures for harmonization [22] |
Key Regulatory Concepts and Recent Developments
FDA's CGMP and Advanced Manufacturing: The FDA's CGMP regulations are the minimum requirements for ensuring drug quality. A January 2025 draft guidance clarifies considerations for in-process controls under 21 CFR 211.110, supporting the use of advanced manufacturing technologies like continuous manufacturing and real-time quality monitoring. The FDA encourages a scientific and risk-based approach for in-process sampling but currently advises that process models should be paired with physical testing, not used alone [24].
EMA's Variations System and Lifecycle Management: The EMA's updated Variations Guidelines, effective in 2025, introduce a more streamlined, predictable system for managing post-approval changes to medicines. The system is based on a risk-based classification (Type IA, IB, and II) and supports modern tools like Post-Approval Change Management Protocols (PACMPs) and Product Lifecycle Management (PLCM) documents. This facilitates faster implementation of changes, benefiting complex products like Advanced Therapy Medicinal Products (ATMPs) [25].
Method Validation According to ICH Q2(R1) Guidelines
The ICH Q2(R1) guideline, "Validation of Analytical Procedures," provides a foundational framework for establishing that analytical methods are suitable for their intended purpose. For pharmaceutical residue analysis, this translates to demonstrating that the method can reliably detect, identify, and quantify residue levels in specific matrices [5] [6].
The core validation parameters mandated by ICH Q2(R1) and their relevance to residue analysis are detailed in the table below.
Table 2: Core ICH Q2(R1) Validation Parameters for Pharmaceutical Residue Analysis
| Validation Parameter | Definition | Application in Residue Analysis |
|---|---|---|
| Accuracy | Closeness of test results to the true value. | Assessed by spiking the matrix with known analyte concentrations and measuring recovery [5]. |
| Precision | Degree of scatter among individual test results. Includes repeatability and intermediate precision. | Critical for ensuring consistent measurement of residue levels across different days, analysts, or equipment [5]. |
| Specificity | Ability to assess the analyte unequivocally in the presence of other components. | Demonstrates the method can distinguish the residue from interfering matrix components, impurities, or degradation products [5]. |
| Limit of Detection (LOD) | Lowest amount of analyte that can be detected. | Important for establishing the method's sensitivity and the threshold for residue presence [5]. |
| Limit of Quantitation (LOQ) | Lowest amount of analyte that can be quantified with acceptable accuracy and precision. | Defines the lower limit of the quantitative range for the residue [5]. |
| Linearity | Ability to obtain test results proportional to analyte concentration. | Established across a range encompassing the expected residue levels [5]. |
| Range | Interval between upper and lower analyte concentrations with suitable precision, accuracy, and linearity. | The validated range must cover all potential residue concentrations from the cleaning or manufacturing process [5]. |
| Robustness | Capacity to remain unaffected by small, deliberate variations in method parameters. | Evaluates method reliability during normal use, e.g., small changes in pH, temperature, or mobile phase composition [5]. |
Experimental Protocol for a Validated Residue Analysis Method
The following workflow provides a generalized protocol for developing and validating an analytical method for pharmaceutical residue analysis, based on ICH Q2(R1) principles and the modernized ICH Q14 on Analytical Procedure Development [5].
Figure 1: Analytical Method Lifecycle Workflow. This diagram outlines the key stages from defining the method's purpose to its ongoing management, aligning with modern ICH Q2(R2) and Q14 guidelines.
Title: Analytical Method Lifecycle Workflow
Protocol Steps:
- Define the Analytical Target Profile (ATP): Before development, prospectively define the method's purpose and the required performance criteria for the residue analysis. This includes the analyte, matrix, required sensitivity (LOD/LOQ), and acceptable levels of accuracy and precision [5].
- Conduct Risk Assessments: Use a systematic, risk-based approach (as described in ICH Q9) to identify and prioritize potential variables that could impact method performance. This guides the robustness studies and informs the overall control strategy [5].
- Develop a Formal Validation Protocol: Create a detailed protocol that specifies the validation parameters to be tested (from Table 2), the experimental design, acceptance criteria (justified by the ATP and risk assessment), and sampling procedures [5].
- Execute the Validation Study: Perform laboratory experiments to collect data for each validation parameter as per the protocol. For residue analysis, this typically involves preparing samples by spiking the specific matrix (e.g., equipment surface swabs, manufacturing components) with known concentrations of the analyte.
- Document and Establish Control Strategy: Compile the data and report the outcome. Justify that the method is validated for its intended use. Define the control strategy, including system suitability tests and procedures for any future method changes [5].
- Lifecycle Management: Implement a procedure for managing post-approval changes to the method. The enhanced approach in ICH Q14 allows for more flexible management of changes through an established control strategy and continued monitoring [5].
The Scientist's Toolkit: Essential Reagents and Materials
Successful method validation and routine analysis require high-quality materials. The following table lists key research reagent solutions and their critical functions in pharmaceutical residue analysis.
Table 3: Essential Research Reagent Solutions for Pharmaceutical Residue Analysis
| Reagent / Material | Function in Analysis |
|---|---|
| Certified Reference Standards | Provides a benchmark of known identity, purity, and strength to calibrate instruments, validate methods, and ensure accuracy [5]. |
| High-Purity Solvents | Used for sample preparation, dilution, and as mobile phase components in chromatography; purity is critical to prevent background interference. |
| Chromatographic Columns | The heart of separation (HPLC/UPLC, GC); critical for achieving specificity and resolving the analyte from matrix components [5]. |
| Sample Preparation Kits | (e.g., Solid-Phase Extraction, Filters) Isolate and concentrate the target residue from the complex sample matrix, improving sensitivity and accuracy. |
| System Suitability Test Solutions | A mixture of analytes used to verify that the chromatographic system is performing adequately at the time of testing, ensuring data integrity [5]. |
Navigating the regulatory landscape for pharmaceutical analysis requires a deep understanding of both the harmonized ICH guidelines and the specific implementations of regional authorities like the FDA and EMA. The core principles of ICH Q2(R1) provide the universal framework for demonstrating that an analytical method is valid and reliable. However, success in global drug development depends on appreciating the nuances of FDA's CGMPs, including their evolving stance on advanced manufacturing, and the EMA's centralized procedures and streamlined variation guidelines.
By integrating a modern, lifecycle approach to method validation—beginning with a clear ATP and supported by robust risk management—scientists can not only meet current regulatory expectations but also build a flexible foundation for continuous improvement. This ensures that pharmaceutical products, supported by rigorously validated analytical data, consistently meet the highest standards of quality, safety, and efficacy for patients worldwide.
Implementing ICH Q2(R1): A Step-by-Step Approach for Residue Methods
Analytical method validation serves as a critical foundation for ensuring the reliability, accuracy, and reproducibility of data in pharmaceutical residue analysis research. This process provides documented evidence that an analytical procedure is suitable for its intended purpose, establishing a foundation of confidence in the results generated during drug development and quality control. For researchers and scientists working with pharmaceutical residues, a properly validated method ensures that trace-level analyses are scientifically sound and defensible, which is particularly important given the complex matrices and low concentration levels often involved.
The International Council for Harmonisation (ICH) Q2(R1) guideline, titled "Validation of Analytical Procedures: Text and Methodology," represents the internationally recognized standard for validating analytical methods. This guideline provides a comprehensive framework that harmonizes requirements across regulatory jurisdictions, ensuring that methods developed in one region will be accepted in others. The validation process under ICH Q2(R1) involves testing a series of performance characteristics to demonstrate that a method consistently produces results that meet predefined acceptance criteria, thereby confirming its fitness for the intended application in pharmaceutical analysis [9].
For the analysis of pharmaceutical residues, which often involves detecting and quantifying trace-level compounds in complex matrices, a rigorous validation protocol is not merely a regulatory formality but a scientific necessity. This article provides a structured comparison of validation approaches according to IICH Q2(R1) guidelines, offering researchers a framework for developing robust validation protocols with clearly defined scope and acceptance criteria tailored to pharmaceutical residue analysis.
Core Validation Parameters and Acceptance Criteria According to ICH Q2(R1)
The ICH Q2(R1) guideline defines eight key validation characteristics that collectively demonstrate an analytical method's suitability for its intended purpose. For pharmaceutical residue analysis, each parameter must be carefully evaluated with acceptance criteria that reflect the method's specific application, whether for identity testing, assay, impurity quantification, or limit testing.
Specificity is the ability of a method to measure the analyte unequivocally in the presence of other components that may be expected to be present in the sample matrix. For pharmaceutical residue analysis, this parameter is crucial as it demonstrates that the method can distinguish and quantify the target residue without interference from excipients, degradation products, or matrix components. Specificity is typically established by comparing chromatograms or spectra of blank matrices with those spiked with the target analyte, demonstrating baseline separation from potential interferents [26] [27].
Accuracy refers to the closeness of agreement between the measured value and the true value. For quantitative methods in residue analysis, accuracy is typically expressed as percent recovery of known amounts of analyte spiked into the matrix. ICH Q2(R1) recommends establishing accuracy across the method's range using a minimum of nine determinations over at least three concentration levels (e.g., three concentrations with three replicates each). Acceptance criteria for accuracy in pharmaceutical analysis generally require mean recovery between 80-120% for impurity methods and 98-102% for assay methods, though these ranges may be justified based on the analytical technique and analyte concentration [27].
Precision encompasses both repeatability (intra-assay precision) and intermediate precision (inter-assay precision). Repeatability expresses the precision under the same operating conditions over a short interval of time, typically demonstrated through multiple measurements of homogeneous samples. Intermediate precision examines the influence of variations such as different analysts, equipment, or days on analytical results. For residue analysis methods, precision is usually expressed as the relative standard deviation (%RSD) of multiple measurements. Acceptance criteria typically require RSD values below 2% for assay methods of drug substances and below 15% for impurity quantification, though these limits must be scientifically justified based on the method's intended use [27].
Detection Limit (DL) and Quantitation Limit (QL) are critical parameters for residue analysis, where trace-level detection is often required. The DL represents the lowest concentration of analyte that can be detected but not necessarily quantified, while the QL is the lowest concentration that can be quantified with acceptable accuracy and precision. These limits can be determined based on visual evaluation, signal-to-noise ratio (typically 3:1 for DL and 10:1 for QL), or the standard deviation of the response and the slope of the calibration curve [27].
Linearity demonstrates the ability of the method to produce results that are directly proportional to analyte concentration within a specified range. Linearity is typically established by preparing and analyzing a series of standard solutions at different concentration levels, then evaluating the correlation coefficient, y-intercept, and slope of the regression line. For chromatographic methods in pharmaceutical analysis, correlation coefficients (r) of ≥0.999 are generally expected for assay methods, while r≥0.995 may be acceptable for impurity methods [27].
Range defines the interval between the upper and lower concentrations of analyte for which the method has suitable levels of accuracy, precision, and linearity. The appropriate range depends on the method's application, with typical recommendations being 80-120% of the target concentration for assay methods, and from the reporting threshold to 120% of the specification for impurity methods [27] [10].
Robustness evaluates the method's capacity to remain unaffected by small, deliberate variations in method parameters, such as pH, mobile phase composition, temperature, or flow rate in chromatographic methods. Robustness testing helps identify critical parameters that must be closely controlled during method execution and establishes system suitability criteria to ensure method performance [27].
Table 1: Core Validation Parameters and Typical Acceptance Criteria for Pharmaceutical Residue Analysis
| Validation Parameter | Experimental Approach | Typical Acceptance Criteria |
|---|---|---|
| Specificity | Compare analyte response in presence of potentially interfering compounds | No interference observed; baseline separation |
| Accuracy | Spike recovery studies at multiple levels | Recovery 80-120% (impurities); 98-102% (assay) |
| Precision | Multiple measurements of homogeneous samples | RSD <2% (assay); <15% (impurities) |
| Linearity | Analyze minimum of 5 concentration levels | Correlation coefficient r ≥ 0.999 (assay); r ≥ 0.995 (impurities) |
| Range | Establish interval where validation parameters are acceptable | 80-120% of test concentration (assay); QL to 120% of spec (impurities) |
| Detection Limit | Signal-to-noise ratio or statistical approach | S/N ≥ 3:1 |
| Quantitation Limit | Signal-to-noise ratio or statistical approach | S/N ≥ 10:1; Accuracy and precision as defined |
Comparative Analysis of ICH Q2(R1) with Other Regulatory Frameworks
While ICH Q2(R1) serves as the international benchmark for analytical method validation, various regional pharmacopeias and regulatory bodies have established their own guidelines with subtle but important differences. Understanding these distinctions is crucial for researchers developing methods intended for global regulatory submissions or comparing performance across different regulatory frameworks.
The United States Pharmacopeia (USP) provides guidance on analytical method validation in General Chapter <1225>, which aligns closely with ICH Q2(R1) but includes terminology differences, such as the use of "ruggedness" instead of "intermediate precision." USP places greater emphasis on system suitability testing (SST) as a prerequisite for method validation and provides more practical examples tailored to compendial methods. For pharmaceutical residue analysis, this focus on system suitability ensures that the analytical system is functioning correctly at the time of analysis, which is particularly important for methods analyzing trace-level compounds where system performance directly impacts data quality [9].
The Japanese Pharmacopoeia (JP) outlines validation requirements in General Information Chapter 17, which closely follows ICH Q2(R1) but with a stronger emphasis on robustness and system suitability testing. JP guidelines may be more prescriptive in certain areas, reflecting Japan's regulatory environment, and may require additional documentation to meet Japanese regulatory standards. For researchers developing methods for pharmaceutical residue analysis that might be submitted in Japan, this heightened focus on robustness warrants additional experimental designs to test method performance under varied conditions [9].
The European Union (EU) guidelines incorporate ICH Q2(R1) into the European Pharmacopoeia (Ph. Eur.) through General Chapter 5.15. While fully adopting ICH principles, the EU provides supplementary guidance for specific analytical techniques, such as chromatography and spectroscopy, and places strong emphasis on robustness testing, particularly for methods used in stability studies. For pharmaceutical residue analysis, this emphasis ensures that methods remain reliable when transferred between laboratories or when slight variations in analytical conditions occur [9].
Table 2: Comparison of Regional Guidelines Based on ICH Q2(R1)
| Regulatory Body | Key Guidance Document | Alignment with ICH Q2(R1) | Unique Emphases |
|---|---|---|---|
| ICH | Q2(R1): Validation of Analytical Procedures | Foundation document | Science- and risk-based approach; global harmonization |
| USP | General Chapter <1225> | Highly aligned | Terminology differences ("ruggedness"); emphasis on system suitability testing |
| JP | General Information Chapter 17 | Highly aligned | Strong emphasis on robustness; may require additional documentation |
| EU | Ph. Eur. General Chapter 5.15 | Fully adopted | Supplementary guidance for specific techniques; emphasis on robustness |
Despite these regional variations, the core principles of ICH Q2(R1) remain the foundation for all major guidelines, ensuring a high degree of global harmonization. All guidelines emphasize the importance of accuracy, precision, specificity, linearity, range, detection limit, quantitation limit, and robustness, and all adopt a risk-based approach that allows for flexibility in validation extent based on the method's intended use [9].
For researchers developing validation protocols for pharmaceutical residue analysis, this harmonization means that a well-designed protocol based on ICH Q2(R1) will generally satisfy the core requirements of other regions, though attention should be paid to specific additional expectations based on the target regulatory markets.
Experimental Design and Protocol Development
Developing a robust validation protocol requires careful planning of experimental designs for each validation parameter. The protocol should clearly define the scope of validation, including the type of method (identification, quantitative impurity testing, limit testing, or assay), the analytical technique, and the specific conditions under which the method will be applied.
For accuracy evaluation in pharmaceutical residue analysis, a typical experiment involves preparing a minimum of nine determinations over at least three concentration levels covering the specified range. For example, for an impurity method, this might include preparations at 50%, 100%, and 150% of the specification level. Each preparation is analyzed, and the recovery is calculated by comparing the measured value to the known spiked value. The results should meet predefined acceptance criteria for accuracy, typically expressed as percent recovery, with tighter limits for assay methods (e.g., 98-102%) and wider but justified limits for impurity methods (e.g., 80-120%) [27].
Precision assessment encompasses both repeatability and intermediate precision. Repeatability is demonstrated by analyzing a minimum of six independent preparations at 100% of the test concentration or multiple determinations at three different concentrations (e.g., 80%, 100%, 120%) covering the specified range. Intermediate precision is evaluated by having different analysts perform the analysis on different days using different instruments, when possible. The precision is expressed as the relative standard deviation (%RSD) of the results, with acceptance criteria typically set at ≤2% for assay methods and ≤15% for impurity methods, though these should be justified based on the analytical requirements [27].
Linearity and range are typically established by preparing a series of standard solutions at a minimum of five concentration levels, ideally evenly spaced across the specified range. The results are plotted as analyte response versus concentration, and statistical calculations are performed to determine the correlation coefficient, y-intercept, and slope of the regression line. The range is derived from the linearity data and represents the interval between the upper and lower concentration levels where the method demonstrates acceptable linearity, accuracy, and precision [27] [10].
Specificity for pharmaceutical residue analysis methods is demonstrated by showing that the method can unequivocally identify and quantify the analyte in the presence of other components that might be present in the sample matrix. This is typically achieved by analyzing blank matrices, matrices spiked with the target analyte, and matrices spiked with potential interferents. For stability-indicating methods, specificity should include demonstration of separation from degradation products generated under stress conditions (e.g., acid, base, oxidation, heat, and light) [27].
Robustness testing involves deliberate variations of method parameters to identify critical factors that affect method performance. For a chromatographic method, this might include variations in flow rate (±10%), mobile phase composition (±2% absolute for organic modifier), column temperature (±5°C), pH (±0.2 units), and detection wavelength (±3 nm). The results of robustness testing inform the system suitability criteria and help define the controlled parameters in the final method [27].
The following workflow diagram illustrates the strategic approach to developing a comprehensive validation protocol:
Validation Protocol Development Workflow
The Scientist's Toolkit: Essential Reagents and Materials
Successful execution of a validation protocol requires carefully selected reagents, reference standards, and analytical materials. The following table outlines essential components for validating methods in pharmaceutical residue analysis:
Table 3: Essential Research Reagent Solutions for Analytical Method Validation
| Reagent/Material | Functional Role | Application Examples |
|---|---|---|
| Certified Reference Standards | Provide traceable quantification and method calibration | System suitability testing; preparation of calibration curves; accuracy studies |
| High-Purity Solvents | Serve as mobile phase components and sample diluents | HPLC mobile phases; sample preparation; extraction procedures |
| Characterized Matrix Blanks | Enable specificity demonstration and background interference assessment | Selectivity studies; accuracy/recovery determinations |
| System Suitability Solutions | Verify chromatographic system performance before analysis | Resolution, efficiency, and reproducibility checks |
| Stable Derivatization Reagents | Enhance detection sensitivity for trace-level analysis | Pre-column or post-column derivatization for improved detection |
Developing a comprehensive validation protocol with clearly defined scope and acceptance criteria is fundamental to establishing reliable analytical methods for pharmaceutical residue analysis. The ICH Q2(R1) guideline provides an internationally harmonized framework for this process, with specific parameters that must be evaluated based on the method's intended purpose. While regional variations exist in implementation through USP, JP, and EU guidelines, the core principles remain consistent, ensuring that validated methods generate scientifically sound and defensible data.
For researchers and drug development professionals, a well-designed validation protocol serves not only as a regulatory requirement but as a scientific demonstration of method reliability. By systematically addressing each validation parameter with appropriate experimental designs and scientifically justified acceptance criteria, analysts can ensure the generation of high-quality data that supports the safety and efficacy assessment of pharmaceutical products. As analytical technologies continue to evolve, the fundamental principles of ICH Q2(R1) remain relevant, providing a stable foundation for method validation while allowing sufficient flexibility to accommodate technological advancements in pharmaceutical analysis.
Within the framework of ICH Q2(R1) validation guidelines, establishing the specificity of an analytical method is paramount to ensuring the accurate and reliable assessment of a drug's identity, potency, and purity throughout its shelf life. For methods detecting pharmaceutical residues and impurities, two experimental approaches stand as critical pillars: forced degradation studies and peak purity assessment. Forced degradation proactively generates potential impurities, while peak purity assessment ensures the analytical procedure can detect and resolve them. This guide objectively compares the performance of established and emerging techniques within these domains, providing a structured evaluation of their capabilities in delivering the specificity required for robust method validation.
Forced Degradation Studies: A Proactive Approach to Stability
Forced degradation studies are an essential, proactive exercise that subjects a drug substance or product to exaggerated stress conditions. The primary objective is to elucidate potential degradation pathways, identify degradation products, and, most critically, demonstrate that the analytical method can reliably separate and quantify the active pharmaceutical ingredient (API) from its degradation products—thus proving its stability-indicating property [28] [29].
Core Stress Conditions and Experimental Protocols
A comprehensive forced degradation study investigates a molecule's vulnerabilities across a range of conditions. The table below summarizes the standard stress conditions, their implementations, and the typical degradation reactions they induce [28] [29] [30].
Table 1: Standard Forced Degradation Stress Conditions and Methodologies
| Stress Condition | Experimental Protocol | Common Degradation Pathways | Key Method Development Insights |
|---|---|---|---|
| Acidic Hydrolysis | Exposure to strong mineral acids (e.g., 0.1-1 M HCl) at elevated temperatures (e.g., 40-80°C) for specified durations [28]. | Cleavage of esters, lactones, acetals, and some amides [28]. | Informs formulation strategy for drugs exposed to stomach acid [28]. |
| Basic Hydrolysis | Exposure to strong bases (e.g., 0.1-1 M NaOH) at elevated temperatures (e.g., 40-80°C) for specified durations [28]. | Degradation of esters, amides, lactones, and carbamates; possible β-elimination [28]. | Reveals sensitivity to alkaline environments or basic excipients [28]. |
| Oxidative Degradation | Treatment with oxidizing agents such as hydrogen peroxide (e.g., 0.1-3%) or radical initiators like AIBN (azobisisobutyronitrile) [28]. | Oxidation of electron-rich groups (phenols, amines, sulfides); N-oxide formation [28]. | Identifies oxidative hotspots; guides antioxidant selection in formulation [28]. |
| Thermal Degradation | Exposure to elevated temperatures (e.g., 70-100°C) in solid state or solution for days to weeks [28] [29]. | Decarboxylation, deamination, cyclization, and rearrangement [28]. | Simulates long-term storage in hot climates; informs packaging needs [28]. |
| Photolytic Degradation | Exposure to UV (320-400 nm) and visible light per ICH Q1B guidelines to simulate sunlight [28] [29]. | Bond cleavage, isomerization, ring rearrangement [28]. | Critical for identifying light-sensitive APIs and selecting protective packaging [28]. |
| Humidity Stress | Exposure to high-humidity conditions (e.g., 75-85% relative humidity) at elevated temperatures [28]. | Hydrolysis, recrystallization of amorphous forms, Maillard reactions [28]. | Assesses need for desiccants and moisture-barrier packaging [28]. |
The general workflow for executing and interpreting forced degradation studies is systematic, as illustrated below.
Diagram 1: Forced Degradation Workflow
Performance Comparison: Small Molecules vs. Biologics
The execution and focus of forced degradation studies differ significantly between small molecule drugs and complex biologics, impacting the choice of analytical techniques.
Table 2: Comparison of Forced Degradation Approaches
| Aspect | Small Molecule Drugs | Biologics (Proteins) |
|---|---|---|
| Primary Degradation Pathways | Hydrolysis, oxidation, photolysis [28]. | Aggregation, deamidation, oxidation, fragmentation, disulfide scrambling [29] [31]. |
| Key Analytical Techniques | Reversed-Phase HPLC with DAD/MS [28]. | Size Exclusion Chromatography (SEC), Ion Exchange Chromatography (IEC), Peptide Mapping, Capillary Electrophoresis (CE-SDS) [29] [31]. |
| Extent of Degradation | Typically 5-15% degradation is considered adequate for method validation [29]. | No fixed percentage; aim is to generate meaningful degradants to challenge methods; aggregation levels of 10-15% may be sufficient [29]. |
| Regulatory Focus | ICH Q1A(R2), Q1B, Q2(R1) [30]. | ICH Q1B, Q2(R1), Q5C, Q6B; case-by-case approach is common [29] [31]. |
| Major Challenge | Ensuring method resolves all degradants from the main peak [28]. | Characterizing a wide variety of heterogeneous variants and complex higher-order structure changes [31]. |
Peak Purity Assessment: Ensuring Chromatographic Resolution
Peak purity assessment is the practice of verifying that a chromatographic peak corresponds to a single chemical entity, free from co-eluting impurities. This is a direct measure of an analytical method's specificity [32] [33].
Established Techniques and Emerging Solutions
The pharmaceutical industry relies on several techniques for peak purity assessment, each with distinct strengths and limitations.
Table 3: Comparison of Peak Purity Assessment Techniques
| Technique | Principle of Operation | Performance Data & Capabilities | Key Limitations |
|---|---|---|---|
| Diode Array Detector (DAD) | Compares UV spectra across a chromatographic peak; spectral similarity is calculated via vector comparison or correlation coefficient [32]. | Detects impurities with dissimilar UV spectra; commercial software provides purity indices (e.g., spectral contrast angle, r²) [32]. | Cannot detect impurities with nearly identical UV spectra (e.g., isomers); low-level impurities may be missed [32] [33]. |
| Mass Spectrometry (MS) | Detects co-eluting substances based on differences in mass-to-charge ratio (m/z) [34] [33]. | High sensitivity and specificity; can provide structural identity via MS/MS [34]. | Cannot differentiate isomers with identical m/z; signal suppression can mask low-level impurities [34] [33]. |
| Two-Dimensional Liquid Chromatography (2D-LC) | Heart-cuts a peak from the 1st dimension and re-chromatographs it in a 2nd dimension with orthogonal separation mechanism [34] [33]. | High resolving power; can separate structurally similar impurities and isomers missed by DAD/MS. A study successfully separated API/impurity mixtures in all 10 test cases [33]. | Method development is complex; requires sophisticated instrumentation; longer analysis times [34]. |
The logical relationship for selecting a peak purity technique based on analytical needs is outlined below.
Diagram 2: Peak Purity Technique Selection
Experimental Protocol: A Standardized 2D-LC Screening Platform for Peak Purity
Recent advancements have led to the development of standardized 2D-LC screening platforms for peak purity, designed to overcome the limitations of DAD and MS [33]. The following protocol provides a general framework.
Objective: To detect co-eluting impurities, including isomers, that are not discernible by DAD or MS. Instrumentation: A 2D-LC system equipped with a switching valve, two pumps, and DAD detection. A ten-port, five-position valve with active solvent modulation (ASM) is recommended [33]. Procedure:
- First Dimension (¹D): The sample is analyzed using the existing 1D method (e.g., C18 column, specific mobile phase and gradient) [33].
- Peak Heart-Cutting: Multiple narrow segments ("heart-cuts") are taken across the width of the target API peak as it elutes from the ¹D column [33].
- Transfer and Modulation: Each heart-cut is transferred to a sample loop and then to the ²D column. ASM is used to reduce the strength of the incoming ¹D eluent, focusing the analytes at the head of the ²D column [33].
- Second Dimension (²D) Separation: The trapped analytes are separated using a fast, orthogonal gradient. To maximize orthogonality while staying in reversed-phase mode, the ²D employs a different stationary phase (e.g., C8, PFP, phenyl-hexyl, HILIC) and/or a different mobile phase pH than the ¹D [34] [33].
- Detection and Analysis: The ²D effluent is monitored by DAD (and optionally MS). A pure ¹D peak will yield a single peak in the ²D, while an impure peak will show multiple resolved peaks [33].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key materials and reagents critical for conducting high-quality forced degradation and peak purity studies.
Table 4: Essential Reagents and Materials for Specificity Studies
| Item | Function/Application | Examples & Notes |
|---|---|---|
| Stress Reagents | To induce specific degradation pathways for method validation [28] [30]. | Hydrochloric Acid (HCl), Sodium Hydroxide (NaOH), Hydrogen Peroxide (H₂O₂). Concentrations typically 0.1-1.0 M [28]. |
| MS-Compatible Mobile Phase Additives | To facilitate LC-MS analysis and 2D-LC-MS peak purity assessment without ion suppression [34]. | Formic Acid, Ammonium Acetate, Ammonium Hydroxide. Preferable to non-volatile additives like TFA and phosphates for MS work [34]. |
| Orthogonal HPLC Columns | To achieve separation of structurally similar impurities and isomers in 2D-LC peak purity analysis [34] [33]. | A screening set for the 2nd dimension may include C18, C8, PFP, Phenyl-Hexyl, Biphenyl, HILIC, and Cyano columns to maximize orthogonality [33]. |
| Photostability Chamber | To conduct controlled photodegradation studies in compliance with ICH Q1B [30]. | Must produce combined visible and ultraviolet (UV, 320-400 nm) output. Exposure levels must be justified and documented [29] [30]. |
Forced degradation studies and peak purity assessment are not merely regulatory checkboxes but are fundamental to developing robust, stability-indicating methods. While traditional techniques like DAD and MS are powerful, the emerging data confirms that 2D-LC provides a superior level of assurance for detecting co-elutions, particularly for challenging impurities like isomers. The choice of technique should be guided by the molecule's complexity and the criticality of the method. A holistic strategy, integrating proactive forced degradation with orthogonal peak purity analysis, delivers the specificity required by ICH Q2(R1) and, ultimately, ensures patient safety and drug product efficacy.
This guide provides a comparative analysis of swab and rinse sampling procedures for cleaning validation in pharmaceutical manufacturing. Recovery studies are central to demonstrating that an analytical method can accurately and precisely detect residue on manufacturing equipment. Framed within the requirements of the ICH Q2(R1) validation guideline, this article details experimental protocols, presents quantitative recovery data, and outlines the critical parameters for designing a study that ensures reliable measurement of active pharmaceutical ingredient (API) residues [35].
In pharmaceutical manufacturing, cleaning validation is mandated by cGMP and FDA regulations to prevent cross-contamination and ensure drug product safety [35]. It demonstrates that a cleaning process consistently removes product and process residues from equipment. A pivotal component of validation is the recovery study, which qualifies the sampling and analytical methods used to detect residues. It confirms that the method accurately (closeness to the true value) and precisely (closeness of repeated measurements) recovers a known amount of analyte spiked onto a surface [36]. The data generated must provide confidence that the residue levels measured during routine monitoring are a true reflection of the cleanliness of the equipment.
Experimental Design for Recovery Studies
A well-designed recovery study investigates the major parameters that influence the efficiency of residue recovery from product contact surfaces.
Key Experimental Parameters
The following parameters should be systematically evaluated [35]:
- Sampling Method: A direct comparison between swab and rinse sampling.
- Surface Material: Representative coupons (e.g., Stainless Steel, PVC, Plexiglas) of equipment surfaces.
- Swab Characteristics: Material, texture, and releasability of fibers.
- Solvent and Extraction: Choice of solvent for wetting the swab and for extracting the analyte from the swab and surface.
- Spiking Technique: Including the concentration of the spike solution and allowing it to dry to simulate process conditions.
Detailed Experimental Protocol
The following protocol, adapted from a published study on Chlordiazepoxide, provides a template for a robust recovery investigation [35]:
- Surface Preparation: Clean surface coupons (e.g., 5cm x 5cm) of Stainless Steel, PVC, and Polyester via ultrasonication in water, rinsing with purified water, and drying.
- Solution Preparation: Prepare a stock standard solution of the target analyte (API) in an appropriate solvent. Dilute to create spiking and standard solutions at known concentrations.
- Surface Spiking: Spike a known volume of standard solution onto a defined area of the surface coupon. Allow the solvent to evaporate at room temperature.
- Swab Sampling:
- Use a validated swab type (e.g., Alpha swabs, Texwipe).
- Wet the first swab with a specified solvent (e.g., purified water).
- Swab the surface systematically: wipe horizontally with one side, flip the swab, and wipe vertically.
- Use a second, dry swab to repeat the process on the same area.
- Place both swabs in a test tube and add extraction solvent (e.g., Methanol and water mix).
- Hand-shake for approximately 2 minutes to desorb the analyte.
- Rinse Sampling:
- After spiking and drying, rinse the surface with a defined volume of rinse solvent (e.g., purified water or a solvent mix).
- Shake the surface in the solvent for approximately 5 minutes to extract the residue.
- Collect the rinse solvent for analysis.
- Analysis by HPLC:
- Instrument: HPLC system with UV-VIS detector.
- Column: C18 column (e.g., 250mm x 4.6mm, 5µm).
- Mobile Phase: Isocratic elution with a mix of methanol and water (60:40).
- Flow Rate: 1.0 mL/min.
- Detection: UV at 254 nm.
- Injection Volume: 5 µL.
The entire process, from sampling to analysis, can be visualized in the following workflow:
Comparative Performance Data: Swab vs. Rinse Sampling
The choice between swab and rinse sampling involves a trade-off, as each method has distinct advantages, disadvantages, and recovery performance depending on the surface material.
Table 1: Comparison of Swab and Rinse Sampling Methods
| Feature | Swab Sampling | Rinse Sampling |
|---|---|---|
| Principle | Direct physical removal from a defined surface area [35]. | Solubilization and recovery of residues from the entire equipment surface [35]. |
| Key Advantage | Targets hardest-to-clean and worst-case locations [35]. | Samples a larger, more representative surface area, including inaccessible systems [35]. |
| Key Limitation | May not be practical for hard-to-reach areas [35]. | Residue must be soluble; dried-on or insoluble residues may not be recovered [35]. |
| Ideal Use Case | Critical, small surface areas in direct contact with the product. | Large surface areas, complex piping, and equipment that cannot be disassembled. |
Quantitative data from recovery studies are essential for method qualification. The table below summarizes example recovery rates for different surface materials.
Table 2: Example Recovery Rates by Surface and Sampling Method [35]
| Surface Material | Sampling Method | Mean Recovery (%) |
|---|---|---|
| Stainless Steel | Swab | 63.88 |
| Polyvinyl Chloride (PVC) | Rinse | 97.85 |
Analytical Method Validation per ICH Q2(R1)
The analytical method used to quantify residues must be validated. The HPLC method cited in the experimental protocol demonstrates key validation parameters [35]:
- Linearity: A correlation coefficient (R²) of 0.9999 across a range of concentrations (e.g., 0.78 to 6.2 µg/mL) demonstrates excellent linearity [35].
- Precision: The precision of an analytical method, expressed as the Relative Standard Deviation (R.S.D.), was successfully demonstrated to be lower than 15% for recovery results at multiple concentration levels [35].
- Sensitivity: The Limit of Detection (LOD) and Limit of Quantitation (LOQ) were determined to be 0.0198 µg/mL and 0.0495 µg/mL, respectively [35].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table lists key materials and reagents required for conducting recovery studies, based on the featured experimental protocol [35].
Table 3: Essential Materials for Recovery Studies
| Item | Function / Description |
|---|---|
| Alpha Swabs (Texwipe) | For mechanically removing residue from a defined surface area; minimal analyte retention and fiber release are critical [35]. |
| Surface Coupons | Representative samples (e.g., 5cm x 5cm) of product contact surfaces (Stainless Steel, PVC, Plexiglas) for controlled recovery experiments [35]. |
| HPLC System with UV Detector | For separation, detection, and quantification of the target analyte at trace levels [35]. |
| USP Reference Standard | Provides a known purity benchmark for the analyte to ensure accurate quantification and method calibration [35]. |
| HPLC-Grade Solvents | High-purity solvents (e.g., Methanol, Water) for mobile phase preparation, sample dilution, and extraction to minimize background interference [35]. |
A scientifically sound recovery study is fundamental to any cleaning validation program. The data presented demonstrates that the choice of sampling method and surface material directly impacts recovery efficiency. Swab sampling is indispensable for assessing critical, localized areas, while rinse sampling provides a broader system-wide profile. A method that integrates both approaches, supported by a validated HPLC analysis that meets ICH Q2(R1) criteria for linearity, precision, and sensitivity, offers the most robust strategy for ensuring equipment cleanliness and patient safety.
Determining Linearity, Range, and Robustness for Residue Assays
In the highly regulated field of pharmaceutical analysis, demonstrating that an analytical method is fit for purpose is paramount. For residue assays, which often quantify low-level impurities or contaminants, establishing Linearity, Range, and Robustness is not merely a regulatory formality but a fundamental requirement for data integrity and product safety [13] [27]. These three parameters, as defined by the ICH Q2(R1) guideline, form an interdependent framework that ensures your method produces reliable, accurate, and meaningful results throughout its lifecycle [11] [37].
This guide provides a detailed, comparative examination of these key validation characteristics, framing them within the practical context of residue analysis for pharmaceutical research and development professionals. We will dissect the regulatory definitions, present experimental protocols, and summarize acceptance criteria, offering a solid foundation for the successful validation of your analytical procedures.
The ICH Q2(R1) guideline provides clear, harmonized definitions for validation parameters. Understanding these definitions is the first step in designing appropriate validation studies [27].
Linearity is the ability of an analytical procedure to obtain test results that are directly proportional to the concentration (amount) of analyte in the sample within a given range [38] [27]. For residue assays, this demonstrates that the method can accurately quantify impurities from low levels near the quantitation limit up to the specification threshold.
Range is the interval between the upper and lower concentrations (amounts) of analyte in the sample (including these concentrations) for which it has been demonstrated that the analytical procedure has a suitable level of precision, accuracy, and linearity [27]. It is intrinsically linked to the proven linearity of the method.
Robustness is a measure of a procedure's capacity to remain unaffected by small, deliberate variations in method parameters. It provides an indication of the method's reliability during normal usage and is typically evaluated during the development phase [13] [37].
The table below summarizes the core objectives and regulatory expectations for each characteristic as applied to residue assays.
Table 1: Comparative Overview of Linearity, Range, and Robustness in Residue Assays
| Characteristic | Primary Objective | Typical Minimum Data Points / Variations | Key Statistical Measures |
|---|---|---|---|
| Linearity [13] [38] | Demonstrate proportional response of the detector to analyte concentration. | A minimum of 5 concentration levels. | Correlation coefficient (r), coefficient of determination (r²), y-intercept, slope of the regression line, residual sum of squares. |
| Range [13] [27] | Define the concentration interval where precision, accuracy, and linearity are acceptable. | Defined by the linearity study; the interval must be specified. | The range is not a statistical measure itself but is validated using data from precision, accuracy, and linearity studies conducted within its boundaries. |
| Robustness [13] [38] | Assess method susceptibility to minor, deliberate parameter changes. | Evaluate the impact of at least 3-5 critical parameter variations. | System suitability test results (e.g., resolution, tailing factor) are compared to confirm they remain within specified limits despite the variations. |
Experimental Protocols and Data Interpretation
A successful validation hinges on well-designed experiments and the correct interpretation of the resulting data. The following protocols are aligned with ICH Q2(R1) expectations and industry best practices.
Protocol for Determining Linearity and Range
The experimental workflow for establishing linearity and range follows a logical sequence from preparation to data analysis, as outlined in the diagram below.
Detailed Experimental Steps:
Solution Preparation: Prepare a series of standard solutions spanning the intended range. For an impurity assay, this typically extends from the Reporting Threshold or Quantitation Limit (LOQ) to at least 120% of the specification level [13] [27]. A minimum of five concentration levels is recommended [38].
Analysis and Data Collection: Analyze each concentration level in triplicate using the prescribed method conditions. Record the analyte response (e.g., peak area in chromatography).
Statistical Analysis and Acceptance Criteria:
- Plot the mean response against the concentration and perform a linear regression analysis [38].
- Calculate the correlation coefficient (r), which should typically be ≥ 0.995 [13] or ≥ 0.999 for assay methods [27].
- Report the y-intercept, slope, and coefficient of determination (r²).
- Critically assess the residual plot (the difference between the calculated and observed values). A random scatter of residuals around zero confirms linearity, while a patterned distribution suggests a non-linear relationship that a simple correlation coefficient might mask [13] [37].
Protocol for Determining Robustness
Robustness testing evaluates the method's resilience to minor, intentional changes in operational parameters. The process involves identifying critical variables, systematically varying them, and assessing the impact.
Detailed Experimental Steps:
Identify Critical Parameters: Select method parameters that are most likely to fluctuate and impact results. For a chromatographic residue assay, this often includes [13] [38]:
- Mobile phase pH (± 0.1-0.2 units)
- Buffer concentration (± 10%)
- Column temperature (± 2-5°C)
- Flow rate (± 0.1 mL/min)
- Detection wavelength (± 2-3 nm)
Experimental Design: Vary one parameter at a time (OFAT) while keeping others constant. A more efficient approach is to use a Design of Experiments (DoE) methodology, which can evaluate multiple factors and their interactions simultaneously [11].
Analysis and Acceptance Criteria: For each variation, analyze a system suitability sample and/or a validated reference standard. The method is considered robust if system suitability criteria (e.g., resolution, tailing factor, theoretical plates) are consistently met despite the variations [13]. The data should demonstrate that the primary output, such as the assay result for the residue, remains unaffected.
Comparative Analysis of Acceptance Criteria
The acceptance criteria for linearity, range, and robustness, while distinct, collectively ensure the method's suitability. The table below provides a consolidated view of typical criteria for a chromatographic residue assay.
Table 2: Summary of Typical Acceptance Criteria for Residue Assays
| Validation Characteristic | Typical Acceptance Criteria | Supporting Data & Calculations |
|---|---|---|
| Linearity [13] [38] [27] | Correlation coefficient (r) ≥ 0.995Visual inspection of residual plot shows random scatter. | Regression line equation (y = mx + c).Calculation of residuals (observed - calculated value). |
| Range [13] [27] | The specified range must demonstrate acceptable precision, accuracy, and linearity. The LOQ must be ≤ the reporting limit for impurities [37]. | The range is validated using precision (RSD) and accuracy (% recovery) data from concentrations at the lower end, middle, and upper end of the range. |
| Robustness [13] [38] | All system suitability test parameters (e.g., resolution, tailing) remain within predefined limits despite deliberate parameter variations. No significant impact on the quantitative result for the residue. | Comparison of key results (e.g., assay value, retention time) obtained under standard and varied conditions. |
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key materials and reagents commonly required for validating linearity, range, and robustness in residue assays, particularly for techniques like HPLC.
Table 3: Essential Research Reagent Solutions for Method Validation
| Item | Function in Validation | Application Example |
|---|---|---|
| Analytical Reference Standard | Serves as the benchmark for preparing calibration solutions to establish linearity and define the range. Its known purity and concentration are critical for accuracy [39]. | Used to prepare the stock and working standard solutions for the linearity experiment. |
| High-Purity Solvents & Buffers | Used to prepare the mobile phase and sample solutions. Consistent quality is vital for achieving reproducible retention times and detector response, directly impacting robustness [39]. | A mixture of water, acetonitrile, and trifluoroacetic acid (TFA) as an ion-pairing agent in RP-HPLC [39]. |
| Chromatographic Column | The stationary phase where separation occurs. Its performance is critical for specificity and can be a key variable in robustness testing (e.g., testing different column batches) [13]. | A wide-pore C8 or C18 column (e.g., 300Å) is often used for the analysis of large biomolecules [39]. |
| System Suitability Test Solution | A reference mixture containing the analyte and any known critical impurities used to verify that the chromatographic system is performing adequately before and during validation experiments [13]. | Injected at the start of a sequence to confirm parameters like plate count and tailing factor are within specified limits. |
The rigorous determination of Linearity, Range, and Robustness is a non-negotiable pillar of analytical method validation for residue assays under ICH Q2(R1). As demonstrated, these parameters are deeply interconnected: a method's proven linearity defines its valid range, while its robustness ensures that linearity and performance are maintained despite minor operational fluctuations. By adhering to the structured experimental protocols and acceptance criteria outlined in this guide, scientists and drug development professionals can generate defensible data that meets global regulatory expectations. This disciplined approach ultimately guarantees the quality, safety, and efficacy of pharmaceutical products by ensuring that impurity levels are monitored with reliable, validated methods.
In pharmaceutical manufacturing, cleaning validation represents a critical quality assurance measure to prevent cross-contamination and ensure patient safety. This process provides documented evidence that cleaning procedures consistently remove residues of Active Pharmaceutical Ingredients (APIs), cleaning agents, and microbial contaminants from manufacturing equipment to predetermined acceptable levels [40]. The selection and validation of cleaning methods for worst-case APIs present particular challenges for pharmaceutical scientists and drug development professionals. These compounds, characterized by poor solubility, high potency, or difficult cleaning properties, establish the minimum threshold for cleaning validation protocols [41]. A scientifically rigorous approach to worst-case API validation ensures that cleaning procedures effective for these challenging compounds will also be effective for less demanding products manufactured on the same equipment [42].
Regulatory guidance from agencies including the FDA, EMA, and ICH emphasizes a risk-based approach to cleaning validation, requiring manufacturers to justify their worst-case selections through systematic scientific assessment [40]. This case study examines the application of a structured framework to cleaning validation for a worst-case API, with specific experimental data and methodology aligned with analytical method validation principles outlined in ICH Q2(R1) guidelines [6]. The framework integrates health-based exposure limits, robust sampling techniques, and validated analytical methods to demonstrate comprehensive contamination control in quality control laboratories [41].
Methodology: A Systematic Framework for Worst-Case API Cleaning Validation
Worst-Case API Selection Criteria
The foundation of an effective cleaning validation program begins with scientifically justified selection of a worst-case API. Research indicates that a systematic approach incorporating multiple risk factors provides the most robust basis for this selection [41]. The proposed methodology employs a multi-parameter assessment to identify the most challenging compound for cleaning processes.
Key selection criteria include:
- API Concentration: Higher potency compounds present greater contamination risks at lower residue levels [41]
- Solubility Profile: APIs with low water solubility present significantly greater cleaning challenges, as they resist removal by aqueous cleaning methods [41] [43]
- Toxicity Considerations: Highly toxic compounds require lower acceptance limits, increasing analytical detection challenges [41]
- Cleaning Difficulty: Historical data on residue persistence and cleaning effectiveness provides practical insights [41]
- Physical and Chemical Properties: Molecular structure, stability, and adhesion properties influence cleanability [43]
This multi-factor approach ensures the selected worst-case API truly represents the most challenging cleaning scenario, providing a conservative benchmark for validation protocols [41].
Experimental Workflow for Cleaning Validation
The following workflow diagram illustrates the systematic approach for conducting cleaning validation studies for worst-case APIs:
Establishing Scientifically Justified Acceptance Criteria
Modern cleaning validation has evolved from traditional approaches to health-based exposure limits, which provide a more scientifically rigorous foundation for establishing acceptance criteria [44]. The Maximum Allowable Carryover (MACO) calculation serves as the cornerstone for determining residue limits:
MACO = (HBEL × MBS × PF) / (TDD × SF)
Where:
- HBEL: Health-Based Exposure Limit (mg/day)
- MBS: Minimum Batch Size for subsequent product
- PF: Purging Factor (specific to API manufacturing)
- TDD: Maximum Therapeutic Daily Dose of subsequent product
- SF: Safety Factor [42]
This approach represents a significant advancement over historical methods, which relied on arbitrary thresholds such as 10 ppm or 1/1000 of the therapeutic dose [44]. Health-based limits, including Acceptable Daily Exposure (ADE) and Permitted Daily Exposure (PDE), incorporate comprehensive toxicological assessment to establish safe residue levels based on the specific pharmacological and toxicological properties of each compound [44].
Sampling Methods and Recovery Studies
Two primary sampling techniques provide complementary data for cleaning validation:
Swab Sampling: Direct surface sampling using polyester swabs pre-wetted with appropriate solvents, systematically applied to 100 cm² areas using horizontal and vertical strokes [41]. This method is particularly effective for flat or irregular surfaces such as large panels and corners [41].
Rinse Sampling: Indirect approach involving equipment rinsing with defined solvent volumes (typically 10 mL total per equipment item) with standardized agitation periods [41]. This method is more suitable for equipment with internal geometries such as pipes and tubes [41].
Recovery studies are critical for validating sampling efficiency, particularly for worst-case APIs with challenging solubility profiles. These studies involve spacing known concentrations of the API onto representative surface coupons, followed by standard sampling and analysis to determine percentage recovery rates [41]. Successful recovery studies typically demonstrate efficiency exceeding 75-80%, ensuring that analytical results accurately reflect surface contamination levels [42] [44].
Case Study Application: Oxcarbazepine as a Worst-Case API
Compound Selection Justification
A recent study demonstrates the practical application of this framework using Oxcarbazepine, an anticonvulsant medication, as a worst-case API [41]. The selection was justified through systematic assessment against established criteria:
Table 1: Worst-Case API Selection Justification for Oxcarbazepine
| Selection Criterion | Oxcarbazepine Profile | Rationale for Worst-Case Designation |
|---|---|---|
| Water Solubility | 0.07 mg/mL at room temperature [41] | Classified as practically insoluble, creating significant cleaning challenges |
| Solubility in Cleaning Solvents | 5.9 mg/mL in acetonitrile; 6.5 mg/mL in acetone at 35°C [41] | Requires specific solvent selection for effective residue removal |
| Toxicity Profile | Established therapeutic agent with defined toxicity [41] | Requires health-based limit calculation for safe residue levels |
| Cleaning History | Documented persistence in cleaning challenges at partner company [41] | Historical evidence of difficult cleaning properties |
| Residue Acceptance Limit | 10 ppm (0.01 mg/mL) established [41] | Aligns with industry standards while presenting analytical challenges |
Experimental Protocol and Parameters
The cleaning validation study employed a comprehensive protocol with the following parameters:
Table 2: Experimental Parameters for Oxcarbazepine Cleaning Validation
| Parameter | Specification | Methodological Justification |
|---|---|---|
| Surface Materials | PVC, Stainless Steel, Polyethylene [44] | Represents common equipment surfaces in pharmaceutical manufacturing |
| Coupon Specifications | 5 cm × 5 cm with surface roughness ≤0.8 μm [44] | Standardized surface area for recovery studies |
| Cleaning Agents | Phosphate-free alkaline detergent (TFD4 PF) for manual cleaning; TFD7 PF for automated cleaning [41] | Environmentally compatible yet effective cleaning agents |
| Analytical Solvents | Acetonitrile and acetone [41] | Optimal solubility characteristics for Oxcarbazepine |
| HPLC Parameters | C8 column (250 mm × 4.6 mm, 5 μm); Mobile phase: 45:55 acetonitrile:water with 0.1% triethylamine and 0.1% trifluoroacetic acid; Flow rate: 0.9 mL/min; Detection: UV 235 nm [44] | Optimized separation and detection for Oxcarbazepine |
| Sampling Method Combination | Swab sampling for accessible surfaces (Petri dishes, spatulas, mortars); Rinse sampling for complex geometries [41] | Comprehensive coverage of equipment surfaces |
Recovery Study Results
Recovery studies demonstrated the efficiency of the selected sampling methods and solvents for Oxcarbazepine residue analysis:
Table 3: Recovery Study Results for Oxcarbazepine Across Different Surfaces
| Surface Material | Recovery Percentage | RSD (%) | Compliance with Acceptance Criteria |
|---|---|---|---|
| Stainless Steel (electropolished) | 78.5% | 4.2 | Meets ≥75% recovery target [44] |
| Polyvinyl Chloride (PVC) | 73.65% | 5.8 | Slightly below but acceptable with justification [44] |
| Polyethylene (PE) | 81.20% | 3.9 | Exceeds recovery target [44] |
| Overall Method Average | 77.78% | 4.6 | Within acceptable variability (RSD <15%) [44] |
The slightly lower recovery on PVC surfaces highlights the importance of surface material consideration in cleaning validation programs, particularly for worst-case APIs with challenging solubility profiles [44].
Analytical Method Validation According to ICH Q2(R1) Guidelines
Validation Parameters and Acceptance Criteria
The analytical method for Oxcarbazepine detection was rigorously validated according to ICH Q2(R1) guidelines [6] [44]. The following table summarizes the validation parameters and results:
Table 4: Analytical Method Validation Parameters for Oxcarbazepine Detection
| Validation Parameter | ICH Q2(R1) Requirement | Experimental Results | Compliance Status |
|---|---|---|---|
| Specificity | No interference from other components | Baseline separation of Oxcarbazepine from potential impurities | Compliant [44] |
| Linearity Range | Minimum 5 concentration points | 7.43 - 87.12 μg/mL (5 points) | Compliant [44] |
| Correlation Coefficient (R²) | Typically ≥0.999 | 0.999997 | Exceeds requirement [44] |
| Accuracy (% Recovery) | Consistent with required precision | 73.65-81.20% across different surfaces | Compliant for cleaning validation [44] |
| Precision (RSD) | RSD <2% for assay methods | RSD ≤5.8% across all recovery studies | Compliant for cleaning validation [44] |
| LOD (Limit of Detection) | Signal-to-noise ratio ≈3:1 | 2.23 μg/mL | Sufficient for 10 ppm limit [44] |
| LOQ (Limit of Quantification) | Signal-to-noise ratio ≈10:1 | 7.43 μg/mL | Sufficient for 10 ppm limit [44] |
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful execution of cleaning validation studies requires specific materials and reagents with defined functions:
Table 5: Essential Research Reagent Solutions for Cleaning Validation Studies
| Item | Specification | Function in Cleaning Validation |
|---|---|---|
| HPLC System with UV Detection | Waters Alliance series or equivalent with C8 column [44] | Separation, identification, and quantification of target API residues |
| Swab Materials | Polyester swabs (e.g., Texwipe 761) [44] | Direct surface sampling for residue recovery |
| Extraction Solvents | Acetonitrile and acetone (HPLC grade) [41] [44] | Dissolution and extraction of API residues from swabs and surfaces |
| Surface Coupons | 316L Stainless Steel, PVC, Polyethylene (5 cm × 5 cm) [44] | Representative surfaces for recovery studies |
| Cleaning Agents | Phosphate-free alkaline detergents (TFD4 PF, TFD7 PF) [41] | Validated cleaning solutions for residue removal |
| Reference Standards | API BPCRS (British Pharmacopoeia Chemical Reference Substance) [44] | Quantification and method calibration |
Results and Discussion: Implications for Pharmaceutical Quality Systems
Statistical Analysis and Data Trending
The validation data for Oxcarbazepine cleaning demonstrates the effectiveness of the systematic approach for worst-case API validation. Statistical analysis of results confirmed method robustness, with relative standard deviation (RSD) values below 15% across all validation parameters, meeting ICH Q2(R1) requirements for precision [44] [27]. Linear regression analysis of the calibration curve yielded a correlation coefficient (R²) of 0.999997, indicating excellent linearity across the validated range [44].
Process capability analysis, using capability indices (Cpk), provides a statistical measure of how effectively the cleaning process meets established acceptance criteria [43]. For cleaning validation, a one-sided upper specification limit (USL) is typically used to calculate Cpk, with values between 1.25 and 2.00 representing optimal process control [43]. Ongoing monitoring and trending of cleaning validation data enables manufacturers to detect unplanned departures from validated processes and implement corrective actions before compliance issues arise [43].
Regulatory and Practical Implications
The case study demonstrates the critical evolution from traditional cleaning validation approaches to modern, risk-based methodologies aligned with regulatory expectations [43]. Health-based exposure limits (HBELs) have largely replaced historical methods such as the "10 ppm rule" or "1/1000 of therapeutic dose" approach, providing more scientifically defensible acceptance criteria [44]. Regulatory bodies including the FDA and EMA increasingly emphasize toxicological risk assessment and quality risk management principles in cleaning validation programs [40].
Recent FDA compliance trends indicate that inadequate cleaning validation studies account for approximately 45% of observations, while missing analytical verification represents 28% of citations [42]. These statistics highlight the importance of robust validation frameworks, particularly for worst-case APIs. The systematic approach outlined in this case study addresses common regulatory deficiencies through comprehensive documentation, scientific justification of worst-case selection, and validated analytical methods with appropriate sensitivity [42].
From a practical implementation perspective, the case study demonstrates that effective cleaning validation for worst-case APIs requires multidisciplinary collaboration involving analytical chemistry, quality assurance, toxicology, and manufacturing expertise [45]. Continuous monitoring programs, rather than periodic revalidation, represent current industry best practices for maintaining the validated state [43]. This approach aligns with the process life-cycle model described in FDA process validation guidance, emphasizing ongoing verification rather than point-in-time validation [43].
This case study demonstrates the successful application of a systematic framework to cleaning validation for a worst-case API, using Oxcarbazepine as a model compound. The integrated approach combines risk-based API selection, health-based acceptance criteria, optimized sampling techniques, and analytical method validation according to ICH Q2(R1) guidelines. Experimental results confirm that the methodology delivers reliable, reproducible data for assessing cleaning effectiveness, with recovery rates of 73.65-81.20% across different surface materials and precision values within acceptable limits (RSD <15%).
The framework provides pharmaceutical researchers, scientists, and drug development professionals with a validated approach for addressing the most challenging cleaning validation scenarios. By establishing a scientifically rigorous foundation for worst-case validation, manufacturers can ensure comprehensive contamination control across their entire product portfolio. The methodology supports regulatory compliance while optimizing resource allocation through risk-based principles, ultimately safeguarding product quality and patient safety in pharmaceutical manufacturing.
Overcoming Challenges in Residue Method Validation and Optimization
Common Pitfalls in Low-Level Residue Analysis and How to Avoid Them
Low-level residue analysis is a critical yet challenging component of pharmaceutical cleaning validation and impurity testing. Method failures at this stage can lead to costly delays, compliance issues, and potential risks to product quality. This guide examines common pitfalls encountered during such analyses and provides a structured, evidence-based comparison of avoidance strategies, all framed within the rigorous context of method validation as per ICH Q2(R1) guidelines.
Understanding the Analytical Landscape and Regulatory Framework
The precision of analytical methods directly influences the safety and efficacy of pharmaceutical products. Method validation is not just a regulatory formality but a cornerstone of quality assurance. The ICH Q2(R1) guideline, "Validation of Analytical Procedures: Text and Methodology," provides a standardized framework for demonstrating that an analytical procedure is suitable for its intended purpose [46]. For low-level residue analysis, this involves validating characteristics such as precision, sensitivity, specificity, and detection and quantitation limits (LOD/LOQ) to ensure accurate and reliable measurement of trace-level contaminants [6].
The challenge intensifies as regulatory expectations evolve. Cleaning validation guidelines from agencies like the FDA, EMA, and Health Canada now require demonstrating that contaminants can be effectively recovered from equipment surfaces, necessitating robust swab recovery studies [47]. Furthermore, the trend towards lower residue limits based on Health-Based Exposure Limits (HBELs) places additional demands on analytical methods, pushing them to their limits of detection and quantitation [48]. Navigating this complex landscape requires a proactive, risk-based approach to method development and validation to prevent the pitfalls that lead to analytical failure.
Common Pitfalls and Comparative Avoidance Strategies
The journey from method development to successful validation is often fraught with obstacles. The table below summarizes the most frequent pitfalls in low-level residue analysis and the proven strategies to avoid them.
Table: Comparison of Common Pitfalls and Corresponding Avoidance Strategies
| Pitfall Category | Common Pitfall | Proven Avoidance Strategy | Key Experimental/Validation Consideration |
|---|---|---|---|
| Swab Recovery | Low or variable recovery rates from equipment surfaces [47]. | Optimize swab parameters: material, solvent, and technique [47]. Prefer swab sampling over rinse sampling where feasible for higher recovery [48]. | Recovery should be >70% with %RSD <15%. Studies must be performed on all product-contact Materials of Construction (MOCs) [47]. |
| Method Sensitivity | Inability to detect or quantify residues at or below the stringent Acceptable Residue Limit (ARL) [48]. | Proactive method development to ensure LOQ is sufficiently below the ARL [48]. Leverage sampling parameters (area, solvent volume) [48]. | Validate LOD/LOQ per ICH Q2(R1). The method's working range must cover from LOQ to at least 125% of ARL [47] [46]. |
| Sample Strategy | Inadequate sampling locations or technique leading to non-representative results [47]. | Adopt an integrated risk-based approach for selecting worst-case locations and products [48]. | Use a standard swab area of 25 cm² for a representative and practical sample size [47]. |
| Lifecycle Management | Treating method validation as a one-time activity, leading to failures upon transfer or with process changes. | Incorporate knowledge from analytical procedure development (ICH Q14) and use a lifecycle management approach [46]. | Suitable data from development studies can be used as part of validation evidence, ensuring method robustness [46]. |
Deep Dive into Swab Recovery Optimization
As highlighted, swab recovery is a major source of variability. The following experimental protocol is critical for generating reliable validation data.
Table: Essential Research Reagent Solutions for Swab Recovery Studies
| Reagent/Material | Function | Best Practice Considerations |
|---|---|---|
| Coupon (MOC) | Represents the equipment surface material for recovery studies. | Start with stainless steel. Perform recovery on a subset of products for other MOCs (e.g., gaskets) to group data scientifically [47]. |
| Swab | The physical device for residue removal from the coupon. | Select a swab material (e.g., polyester, cotton) that does not interfere with the analyte and provides good mechanical recovery [47]. |
| Swab Solvent | Liquid used to wet the swab to dissolve and recover the residue. | The solvent must effectively dissolve the analyte without causing degradation. Compatibility with the analytical method (e.g., HPLC) is crucial [47]. |
| Extraction Solvent | Liquid used to extract the residue from the swab after sampling. | The solvent should fully recover the analyte from the swab material. Extraction time and method (e.g., sonication, shaking) must be validated [47]. |
Experimental Protocol for Swab Recovery Studies:
- Coupon Preparation: Obtain coupons of all relevant product-contact MOCs. Clean and verify they are free of interfering contaminants.
- Spiking: Spike coupons with the analyte (API, detergent) at known concentrations. Key levels include:
- 125% of ARL: To ensure accuracy above the failure level.
- 100% of ARL: The critical failure point.
- 50% of ARL: A level within the controlled range.
- LOQ: To challenge the method's lower limit [47].
- Recovery Process: Perform recovery in triplicate for each level. Use a validated technique (e.g., a template for a 25 cm² area) to swab the surface with the wetted swab [47].
- Extraction: Place the swab in the extraction solvent and employ a validated method (e.g., sonication for 15 minutes) to extract the residue.
- Analysis: Analyze the extracted samples using the candidate analytical method (e.g., HPLC-UV).
- Calculation & Acceptance: Calculate the percent recovery for each spike. The average recovery across the levels should ideally be ≥70% with a %RSD of ≤15%. Investigate and optimize parameters if recoveries are consistently low or exceed 105% [47].
Workflow for a Robust Residue Analysis Method
The following diagram illustrates the logical workflow for developing and validating a robust low-level residue analysis method, integrating proactive development with formal validation.
Diagram: Residue Analysis Method Workflow
Avoiding failures in low-level residue analysis is achievable through a science-driven, risk-based methodology. The strategies outlined—from optimizing swab recovery parameters and ensuring method sensitivity aligns with HBEL-based limits to adopting a holistic lifecycle approach—provide a robust framework for success. By integrating these practices with the formal validation requirements of ICH Q2(R1), researchers and drug development professionals can build quality into their analytical procedures, ensuring regulatory compliance and, most importantly, safeguarding patient safety.
In the pharmaceutical industry, cleaning validation is a critical regulatory requirement to prevent cross-contamination and ensure product safety. It provides documented evidence that cleaning procedures effectively remove active pharmaceutical ingredients (APIs), cleaning agents, and microbial residues from manufacturing equipment [35] [49]. Within this framework, selecting appropriate sampling techniques is paramount for accurate residue detection and quantification. The two primary sampling methods—swab (direct) and rinse (indirect) sampling—serve complementary yet distinct roles in comprehensive cleaning validation protocols [35] [50].
Swab sampling involves physically wiping a defined surface area with a swab to recover residues, making it particularly suitable for hard-to-clean locations, irregular surfaces, and equipment with complex geometries [49] [50]. This method allows for targeted sampling of worst-case locations that are most difficult to clean, providing a direct measurement of residue per unit surface area [51] [35]. In contrast, rinse sampling utilizes a liquid solvent to rinse the entire equipment surface, effectively integrating residue levels over a large and sometimes inaccessible surface area [51] [50]. This makes it ideal for sampling large or complex equipment systems, including transfer pipework and systems that cannot be routinely disassembled [35] [50].
The recovery efficiency of each method—defined as the percentage of residue successfully recovered and detected from a contaminated surface—is influenced by multiple factors. These include the nature of the residue, surface characteristics, swab material, solvent selection, and operator technique [35] [49]. Establishing validated recovery rates for both swab and rinse methods is essential under ICH Q2(R1) guidelines, as these rates ensure that the analytical methods consistently yield reliable results that reflect the true level of contamination on equipment surfaces [8] [52].
Theoretical Foundations: Principles of Swab and Rinse Sampling
Swab Sampling Mechanics
Swab sampling operates on the principle of mechanical removal where residues are physically dislodged from equipment surfaces through the wiping action of the swab [49]. The effectiveness of this process depends on the swab material's ability to both dislodge and retain residue particles. Polyester, foam, and flocked swabs are commonly used, with flocked swabs often providing superior recovery for low-residue environments due to their enhanced surface contact and absorption properties [49]. The sampling procedure typically involves pre-moistening the swab with an appropriate solvent to dissolve and solubilize the residue, followed by systematic wiping of a defined area using horizontal, vertical, and diagonal strokes to maximize recovery [49] [53]. The swab is then transferred to a container with extraction solvent, where residues are desorbed for analysis [53].
The key advantage of swab sampling lies in its ability to target specific worst-case locations such as corners, seams, and other difficult-to-clean areas that might harbor higher residue levels [51]. This targeted approach makes swab sampling potentially more rigorous for validation purposes, as it is more likely to detect localized contamination that might be diluted in a rinse sample [51]. However, this method requires careful technique standardization and operator training to ensure consistent recovery rates, as variations in pressure, pattern, or angle can significantly impact results [49].
Rinse Sampling Dynamics
Rinse sampling functions through the solubilization and dissolution of residues from equipment surfaces into the rinse solvent [35] [50]. This method assumes that residues are soluble in the chosen solvent and that the rinsing process effectively removes them from all contact surfaces. The rinse sample can be collected either as a grab sample of the final process rinse or through a separate sampling rinse performed specifically for monitoring purposes after cleaning completion [51]. The latter approach provides a more direct assessment of surface cleanliness but requires additional processing steps.
The primary strength of rinse sampling is its ability to access large surface areas and complex equipment geometries that would be impractical to swab [35] [50]. By integrating residue levels across the entire rinsed surface, rinse sampling provides an overall cleanliness assessment rather than localized data [51]. This comprehensive coverage, however, comes with a significant limitation: insoluble or poorly soluble residues may not be effectively recovered, leading to potentially underestimated contamination levels [35] [54]. Additionally, the dilution effect of the rinse volume means that rinse sampling may not detect localized contamination if the overall residue level across all surfaces remains below the detection limit [51].
Table: Comparative Principles of Swab and Rinse Sampling
| Parameter | Swab Sampling | Rinse Sampling |
|---|---|---|
| Sampling Principle | Mechanical removal and absorption | Solubilization and dissolution |
| Surface Coverage | Targeted, specific locations (typically 25-100 cm²) | Comprehensive, entire equipment surface |
| Best Applications | Worst-case locations, irregular surfaces, insoluble residues | Large equipment, complex geometries, transfer lines |
| Key Limitations | Operator-dependent, limited to accessible areas | May miss localized contamination, requires soluble residues |
| Data Provided | Residue per unit area (e.g., μg/cm²) | Total residue in equipment (e.g., μg/mL) |
Method Validation Within ICH Q2(R1) Framework
The International Council for Harmonisation (ICH) Q2(R1) guideline, titled "Validation of Analytical Procedures: Text and Methodology," provides the foundational framework for validating analytical methods used in pharmaceutical analysis, including those for cleaning validation [8]. This guidance outlines key validation parameters that must be established to demonstrate that an analytical procedure is suitable for its intended purpose. For both swab and rinse sampling methods, validation under ICH Q2(R1) requires rigorous assessment of multiple performance characteristics to ensure reliable residue detection and quantification [52].
Specificity is crucial and demonstrates that the method can unequivocally identify and quantify the analyte in the presence of other components such as sampling materials, cleaning agents, or equipment extractables [55] [52]. For swab sampling, this includes testing for interference from the swab material itself [55]. Linearity and range establish that the method produces results directly proportional to analyte concentration within a specified range, which should encompass the residue acceptance limit (RAL) [35] [52]. The limit of detection (LOD) and limit of quantitation (LOQ) determine the lowest levels of residue that can be reliably detected and quantified, with LOQ particularly important for establishing the sensitivity required to detect residues at or below the RAL [35] [52].
Accuracy, expressed as percentage recovery, is perhaps the most critical parameter for sampling methods [52]. Recovery studies involve spiking known amounts of analyte onto representative surfaces and determining the percentage successfully recovered through the sampling and analysis process [35] [52]. Acceptance criteria for recovery typically range from 70-130% for swab sampling and should be consistent across multiple concentration levels [52]. Precision encompasses both repeatability (multiple samples by the same analyst) and intermediate precision (different days, analysts, or equipment), with relative standard deviation (RSD) generally expected to be ≤15% for precision at each concentration level [35] [52].
Diagram: ICH Q2(R1) Validation Parameters for Sampling Methods. This workflow illustrates the key validation parameters required by ICH Q2(R1) guidelines that apply to both swab and rinse sampling methods.
Experimental Recovery Comparison Data
Recovery Rates Across Surface Types
Comparative studies demonstrate significant variability in recovery efficiency between swab and rinse methods depending on surface material and residue solubility. Research examining recovery rates for various pharmaceutical compounds across different surfaces revealed that swab sampling generally provides more consistent recovery for non-soluble compounds, while both methods perform well with soluble residues [35] [54]. A study evaluating chlordiazepoxide recovery reported swab sampling recovery rates of 63.88% for stainless steel surfaces, while rinse sampling achieved 97.85% recovery for PVC surfaces, highlighting how both surface material and sampling method interact to affect recovery efficiency [35].
The solubility of the residue fundamentally impacts method selection. Research on water-insoluble substances like Gentashin ointment demonstrated dramatically different recovery patterns between methods, with rinse sampling recovering less than 20% and swab sampling with water extraction recovering less than 10% of the applied residue [54]. However, when using swab sampling with direct combustion (bypassing extraction difficulties), recovery rates improved to nearly 100% for all substances regardless of solubility [54]. This underscores the critical importance of matching both sampling and analytical techniques to the physicochemical properties of the target residue.
Table: Experimental Recovery Rates for Different Surfaces and Compounds
| Surface Type | Compound | Swab Recovery (%) | Rinse Recovery (%) | Reference |
|---|---|---|---|---|
| Stainless Steel | Chlordiazepoxide | 63.88 | - | [35] |
| PVC | Chlordiazepoxide | - | 97.85 | [35] |
| Stainless Steel | Tranexamic Acid (soluble) | ~95 | ~95 | [54] |
| Stainless Steel | Isopropylantipyrine (insoluble) | ~90 | ~90 | [54] |
| Stainless Steel | Gentashin Ointment (very insoluble) | <10 | <20 | [54] |
| Stainless Steel | Various (with direct combustion) | ~100 | - | [54] |
Impact of Residue Solubility on Recovery
Residue solubility fundamentally dictates the appropriate sampling methodology. Water-soluble compounds such as tranexamic acid and anhydrous caffeine demonstrate high recovery rates with both swab and rinse methods, typically exceeding 90% in controlled studies [54]. This makes method selection less critical for highly soluble residues, allowing flexibility based on equipment geometry and accessibility. However, for water-insoluble compounds like ointments, swab sampling with appropriate solvent selection becomes essential for accurate recovery quantification [54].
Advanced analytical techniques can mitigate solubility challenges. The comparison of extraction methods for swab samples revealed that direct combustion of swabs following sampling achieved nearly 100% recovery for all compounds regardless of solubility, while liquid extraction methods showed poor recovery for insoluble substances [54]. This suggests that for difficult-to-dissolve residues, alternative analytical techniques that bypass solubility limitations may provide more accurate contamination assessment.
Detailed Experimental Protocols
Swab Sampling Protocol
The following protocol outlines a standardized approach for swab sampling recovery studies based on established methodologies [35] [49] [53]:
Surface Preparation: Select representative surface coupons (e.g., stainless steel 316L, PVC, glass) with dimensions of at least 5cm×5cm. Clean surfaces thoroughly using ultrasonication in water, rinse with purified water, and dry at room temperature before use [35].
Surface Spiking: Prepare a standard solution of the target analyte at known concentrations. Using a calibrated micropipette, apply a precise volume (typically 100μL) of the standard solution onto the prepared surface coupon, ensuring even distribution across a defined area (e.g., 25cm² or 100cm²) [35] [52]. Allow the solvent to evaporate completely under ambient conditions.
Swab Selection and Preparation: Select appropriate swab material based on recovery studies (common choices include polyester Texwipe Alpha swabs or flocked swabs). Pre-moisten the swab with a compatible solvent that effectively dissolves the analyte, then remove excess solvent by gentle squeezing [49] [53].
Sampling Technique: Using a sampling template to define the area, systematically wipe the spiked surface with the moistened swab. Employ a standardized pattern: first horizontally with one side of the swab, then vertically with the other side, applying consistent pressure throughout [49] [53]. For optimal recovery, use a second (dry) swab to repeat the process on the same area [35].
Sample Extraction: Place both swabs in a suitable container and add a precise volume of extraction solvent. Seal the container and employ appropriate extraction techniques such as hand shaking for 2 minutes, sonication for 10 minutes, or stirring for 1 hour, depending on the analyte's solubility characteristics [35] [53] [52].
Analysis: Filter the extract if necessary (using 0.45μm syringe filters) and analyze using validated analytical methods such as HPLC, TOC, or UV spectrophotometry [49] [52].
Diagram: Swab Sampling Experimental Workflow. This protocol outlines the key steps for conducting recovery studies using swab sampling methodology.
Rinse Sampling Protocol
The following protocol describes a standardized approach for rinse sampling recovery studies:
Equipment Preparation: Select representative equipment or surface coupons. Clean thoroughly and dry before spiking to prevent interference from pre-existing contaminants [35].
Surface Spiking: Apply a known amount of the target analyte to the internal surfaces of the equipment or to surface coupons representing the equipment material. For equipment with complex geometry, ensure even distribution across representative surfaces, including worst-case locations [35] [54].
Drying: Allow the applied solution to dry completely under ambient conditions to simulate processed residue conditions [35].
Rinsing Procedure: Add a precise volume of rinse solvent to the equipment. For comparative studies, use consistent volumes relative to surface area. Employ appropriate agitation methods such as stirring, swirling, or pumping to ensure complete surface contact [54]. Standardize contact time (typically 15 minutes) and agitation intensity across experiments [54].
Sample Collection: Collect the entire rinse volume or a representative aliquot. For equipment sampling, ensure the collection vessel is clean and compatible with the analyte [35].
Analysis: Analyze the rinse solution directly or with appropriate pretreatment (such as filtration) using validated analytical methods [52]. For non-soluble residues, consider alternative detection methods that address solubility limitations [54].
Recovery Calculation: Calculate percentage recovery by comparing the detected amount to the originally applied amount, accounting for any dilution factors [54] [52].
Essential Research Reagent Solutions
The following reagents and materials are essential for conducting robust recovery studies for both swab and rinse sampling methods:
Table: Essential Research Reagents and Materials for Recovery Studies
| Reagent/Material | Function | Selection Considerations |
|---|---|---|
| Reference Standard | Provides known purity material for spiking and calibration | Use USP/EP grade where available; characterize purity and identity [52] |
| Swabs | Physical removal and retention of residues from surfaces | Consider material (polyester, foam, flocked), size, solvent compatibility; Texwipe Alpha swabs are commonly used [35] [49] |
| Extraction Solvents | Dissolution and extraction of residues from swabs or surfaces | Select based on analyte solubility (water, acetonitrile, acetone, methanol-water mixtures) [35] [53] |
| Rinse Solvents | Dissolution and removal of residues from equipment surfaces | Choose based on analyte solubility and equipment compatibility; purified water is most common [54] |
| Surface Coupons | Representative surfaces for recovery studies | Use actual equipment materials (stainless steel 316L, PVC, glass, etc.) [35] |
| HPLC-grade Mobile Phases | Chromatographic separation and analysis | Ensure compatibility with analyte and column; degas before use [35] [52] |
| TOC Standards | Calibration for total organic carbon analysis | Use potassium hydrogen phthalate or similar certified standards [54] |
Strategic Method Selection and Optimization
Decision Framework for Method Selection
Choosing between swab and rinse sampling requires systematic consideration of multiple factors. Equipment geometry fundamentally influences method selection; swab sampling is preferable for accessible worst-case locations, while rinse sampling is necessary for complex or inaccessible equipment [51] [50]. Residue characteristics equally impact this decision; soluble residues work well with either method, while insoluble residues favor swab sampling with appropriate solvents or direct combustion analysis [54]. The purpose of data also guides selection; swab sampling provides localized, specific data for validation rigor, while rinse sampling gives overall equipment cleanliness assessment [51] [35].
A hybrid approach often provides the most comprehensive validation. Regulatory guidance suggests that a combination of both methods is generally most desirable, with swab sampling targeting worst-case locations and rinse sampling providing overall confirmation [35]. This integrated strategy balances the rigorous, localized assessment of swab sampling with the comprehensive coverage of rinse sampling, effectively addressing the limitations of each method when used in isolation [35] [50].
Optimization Strategies for Enhanced Recovery
Several evidence-based strategies can significantly improve recovery rates for both sampling methods. For swab sampling, optimization includes solvent selection based on analyte solubility studies, swab material evaluation through comparative recovery testing, and comprehensive operator training to ensure technique consistency [49] [53]. For challenging residues, implementation of a double-swab technique (using both moistened and dry swabs) can improve overall recovery [35]. For rinse sampling, optimization strategies include solvent volume adjustment to ensure adequate coverage without excessive dilution, incorporation of mechanical action through increased flow rates or pulsed rinsing, and temperature optimization to enhance solubility without promoting degradation [54].
Advanced analytical techniques can overcome inherent method limitations. For swab sampling with insoluble residues, direct combustion methods coupled with TOC analysis can achieve near-complete recovery regardless of solubility characteristics [54]. For rinse sampling, method sensitivity can be enhanced through sample pre-concentration techniques or utilization of more sensitive detection technologies that lower detection limits [52].
Swab and rinse sampling methods offer complementary approaches for recovery studies in pharmaceutical cleaning validation, each with distinct advantages and limitations. Swab sampling provides superior capability for targeted assessment of worst-case locations and insoluble residues, while rinse sampling offers comprehensive coverage of large and complex equipment systems. The recovery efficiency of each method is influenced by multiple factors including residue solubility, surface characteristics, solvent selection, and operator technique.
Method selection should be guided by a systematic framework considering equipment geometry, residue properties, and the purpose of data collection. Under the ICH Q2(R1) validation framework, both methods require rigorous validation of specificity, linearity, accuracy, precision, and detection limits to ensure reliability [8] [52]. Optimization strategies, including solvent selection, technique refinement, and implementation of advanced analytical approaches, can significantly enhance recovery rates for both methods.
For comprehensive cleaning validation protocols, a combined approach utilizing both swab and rinse sampling often provides the most robust assessment of equipment cleanliness [35]. This integrated strategy leverages the strengths of each method while mitigating their individual limitations, ultimately providing higher assurance of cleaning effectiveness and regulatory compliance.
Strategies for Improving Sensitivity and Dealing with Matrix Interferences
For researchers and drug development professionals working on pharmaceutical residue analysis, the dual challenge of achieving sufficient method sensitivity while effectively managing matrix interferences is a critical aspect of method validation under ICH Q2(R1) guidelines. The accuracy, precision, and reliability of an analytical method directly depend on how well these challenges are addressed during method development and validation. Matrix effects can significantly impact method performance by altering analyte detection and quantification, leading to potential inaccuracies in assessing the identity, potency, quality, and purity of pharmaceutical substances [56]. Simultaneously, inadequate sensitivity can compromise the ability to detect and quantify low-level residues, potentially affecting drug safety profiles. This guide examines proven strategies for enhancing sensitivity and controlling matrix interferences, providing experimental data and practical protocols to support robust method validation compliant with regulatory standards.
Theoretical Foundations: Sensitivity and Matrix Effects
In chromatographic analysis, sensitivity refers to the ability of an method to detect and quantify low concentrations of an analyte, typically measured through the signal-to-noise ratio or the limit of detection (LOD). Matrix interferences occur when other components in the sample co-elute with or affect the detection of target analytes, leading to inaccurate integration, quantification errors, and potential method failure [56] [57]. These interferences originate from various sources, including sample constituents, reagents, solvents, and equipment, and their impact must be thoroughly evaluated during method validation to ensure specificity and selectivity as required by ICH Q2(R1) [56].
The relationship between sensitivity and matrix effects is often inverse; as sensitivity increases to detect lower analyte levels, the method becomes more susceptible to matrix interferences. This balance must be carefully managed through systematic optimization of analytical parameters. Proper integration of chromatographic peaks is particularly crucial, as any error in measuring peak size will produce subsequent errors in reported results, compromising method validity [58].
Figure 1: Analytical Method Optimization Framework
Experimental Comparison of Integration Methods
Methodology for Integration Comparison
A systematic experimental study was conducted to evaluate integration methods for peak separation and quantification. The study employed an Agilent 1100 HPLC system with a C18 column (100 mm × 4.6 mm, 5-μm particles) maintained at 40°C. Test solutions contained nitrobenzene and dimethyl phthalate in acetonitrile, with mobile phases of varying acetonitrile concentrations (45.0%, 67.5%, 75.0%, and 83.0%) in water to achieve resolutions of 4.0, 2.0, 1.5, and 1.0 between analytes. Triplicate injections were performed for each test solution, and all separations were integrated using four baseline methods: drop, valley, exponential skim, and Gaussian skim, with both area and height measurements [58].
Single-component solutions at highest (100%) and lower (5%) concentrations served as calibration references. Analysis at resolution 4.0 defined "true" values for test solutions, with the largest peak assigned a value of 100. Response factors were calculated from the ratio between each component in test solutions and corresponding calibration references, enabling calculation of expected peak responses under each resolution condition. Percent error between observed and expected values was calculated for each integration method [58].
Quantitative Results: Integration Method Performance
Table 1: Integration Method Performance Across Resolution Conditions
| Integration Method | Peak Size Measurement | Resolution 1.5 Error (%) | Resolution 1.0 Error (%) | Optimal Application |
|---|---|---|---|---|
| Drop | Area | +2.1 to -3.5 | +15.8 to -12.3 | Well-resolved peaks (R > 1.5) |
| Drop | Height | +1.3 to -2.1 | +5.4 to -8.7 | Poorly resolved peaks |
| Valley | Area | -12.5 to -18.7 | -25.3 to -31.6 | Baseline-separated peaks only |
| Valley | Height | -8.9 to -14.2 | -18.7 to -26.4 | Not recommended for quantitation |
| Exponential Skim | Area | -5.8 to -25.3* | -15.7 to -42.6* | Shoulder peaks on tailing edge |
| Exponential Skim | Height | -3.2 to -18.4* | -9.8 to -31.5* | Limited applications |
| Gaussian Skim | Area | +1.8 to -4.2 | +8.7 to -10.9 | Shoulder peaks of all types |
| Gaussian Skim | Height | +0.9 to -2.8 | +3.4 to -6.3 | Complex peak separations |
Note: Significant negative errors particularly affect the shoulder peak [58]
The data demonstrates that drop and Gaussian skim methods produce the least error across all resolution situations, while the valley method consistently produces negative errors for both peaks. The exponential skim method generates significant negative error for the shoulder peak. Peak height measurement generally proves more accurate than peak area, particularly for poorly resolved peaks, though this approach has not been widely adopted in practice despite recommendations in the literature [58].
For situations where the smaller peak is at least 5% of the larger peak, resolution greater than 1.5 is necessary to minimize integration errors. Resolution below 1.0 generates unacceptable errors regardless of integration method selected. These findings have significant implications for method validation, as integration errors directly impact accuracy and precision measurements required by ICH Q2(R1) [58].
Systematic Approaches to Improve Sensitivity
Detector Optimization Strategies
Detector parameter optimization represents a crucial approach for enhancing method sensitivity. For UV-Vis detectors, wavelength should be selected by evaluating the absorption spectrum of target analytes to identify the wavelength providing highest absorption, thereby minimizing interference and maximizing sensitivity [59]. Data acquisition rate must be optimized to ensure sufficient data points are collected across each peak; a minimum of 20 data points per peak is required, with 30-40 points ideal for optimal peak resolution and reproducibility [59].
Detector response time should be set according to a specific rule: the response time should equal approximately one-third of the peak width at half the height of the narrowest peak of interest. This parameter optimization ensures accurate peak representation without excessive smoothing that could reduce apparent peak height and compromise sensitivity for low-level analytes [59].
Injection volume optimization must balance sensitivity requirements with chromatographic integrity. As a rule of thumb, injection volume should be 1-2% of the total column volume for sample concentrations of 1μg/μl. Excessive injection volume causes mass overload, leading to peak fronting, decreased retention time, and reduced column efficiency and resolution [59].
Flow rate adjustment provides another sensitivity optimization parameter. Lower flow rates generally decrease the retention factor at the column outlet, making peaks narrower and improving response factor. Conversely, higher flow rates can cause peak widening, decreasing resolution but shortening run time. Columns packed with smaller particles and/or solid-core particles provide benefits in maintaining high peak resolution at faster flow rates [59].
Column temperature management affects both sensitivity and separation efficiency. Higher temperatures allow faster flow rates and quicker analysis but can cause sample degradation and lower resolution. Lower column temperatures increase retention, potentially improving peak resolution but extending analysis time. Temperature limits for sample, solvent, column, and instrumentation must be observed during optimization [59].
Comprehensive Management of Matrix Interferences
Source Identification and Control
Matrix interferences in liquid chromatography originate from three primary sources: reagents/solvents, preparation equipment, and the HPLC system itself. Water quality is a frequently overlooked source of interference peaks, particularly for detection methods employing low wavelengths, where high-quality water is essential to avoid issues caused by water impurities. Various salts can also contribute to chromatographic interference; for example, potassium dihydrogen phosphate has been shown to introduce interference peaks at specific retention times [57].
Equipment used during mobile phase and sample preparation represents another contamination source. Filter membranes can introduce interference peaks, particularly when filtering pure organic phases like methanol or acetonitrile. Plasticware including pipette tips, disposable straws, and syringes are chemically less inert compared to glassware and more likely to introduce interference peaks, especially when detecting at low wavelengths such as 210 nm [57].
The HPLC system itself can be a source of interference through three main mechanisms: strongly retained substances, ion-pair contamination, and bacterial growth. Strongly retained substances not eluted in the current injection may carry over into subsequent injections, appearing as broad peaks during isocratic elution or in high organic phase during gradient elution. Ion-pair reagent contamination typically occurs due to incomplete system washing after using mobile phases containing these reagents, manifesting as increased baseline noise or interference peaks. Bacterial growth in water-phase tubing can surprisingly occur even in HPLC systems, gradually appearing as interference peaks during gradient elution [57].
Strategic Solutions for Interference Reduction
Table 2: Matrix Interference Sources and Mitigation Strategies
| Interference Category | Specific Sources | Impact on Analysis | Recommended Solutions |
|---|---|---|---|
| Reagents & Solvents | Water impurities, Salt contaminants, Filtered organic solvents | Extra peaks, Elevated baseline, Altered retention | Use high-purity water, Install ghost peak trapping column, Avoid re-filtering chromatography-grade solvents |
| Preparation Equipment | Filter membranes, Plastic pipettes/syringes, Improperly cleaned glassware | Introduction of contaminant peaks, Variable retention times | Establish cleaning protocols, Use glass where possible, Verify cleaning effectiveness |
| HPLC System Issues | Strongly retained substances, Ion-pair reagent residue, Bacterial growth in tubing | Peak carryover, Baseline drift, Ghost peaks | Extend elution time, Implement rigorous washing protocols, Flush water channels with organic solvent daily |
| Sample-Related | Degradation products, Sample matrix components, Impurities | Peak co-elution, Signal suppression/enhancement, Integration errors | Optimize sample preparation, Use selective extraction, Employ internal standards |
For interference peaks caused by water and inorganic salts, installing a ghost peak trapping column can effectively prevent such interferences. When using ion-pairing reagents, a ghost peak trapping column that does not affect the ion-pairing reagent should be selected [57].
Strongly retained substances can be eliminated by extending the collection time or increasing the elution strength to prevent interference with subsequent samples. Bacterial growth in the system, while unexpected, can be resolved by flushing the channel containing pure water with an organic solvent at the end of each day [57].
Sample preparation optimization represents the first line of defense against matrix interferences. Proper filtration or extraction based on application and system requirements removes particulates and impurities that would otherwise compromise resolution. For light-sensitive analytes, selecting proper actinic vials prevents analyte degradation, while for hydrophobic/hydrophilic analytes, containers that prevent unwanted binding to surfaces should be selected [59].
Method Validation in Pharmaceutical Analysis
ICH Q2(R1) Compliance Considerations
Method validation according to ICH Q2(R1) guidelines provides definitive evidence that an analytical procedure attains the necessary levels of precision, accuracy, and reliability for its intended application. In the pharmaceutical industry, method validation is indispensable for demonstrating the quality, consistency, and dependability of pharmaceutical substances, thereby protecting consumer safety [56].
The FDA requires data-based proof of the identity, potency, quality, and purity of pharmaceutical substances and products. To avoid negative audit results and penalties, a method must support reproducible results. Common audit deficiencies include methods used in critical decision-making that have not undergone proper validation, method validation that does not yield sufficient data, and poorly controlled method validation processes [56].
Validation Challenges and Solutions
Sample complexity presents significant validation challenges, as the nature and number of sample components may cause method interference, ultimately lowering precision and accuracy. Factors that could affect method performance, such as the impact of degradation products, existence of impurities, and variations in sample matrices, must be evaluated during method validation [56].
Equipment and instrumentation considerations include the use of chromatography instrumentation (GC, HPLC) and mass spectrometry for identifying and quantifying sample compounds. Liquid chromatography and mass spectrometry validation sometimes experience issues with matrix substances that may cause ionization suppression or enhancement in the mass spectrometer [56].
Figure 2: Method Validation Framework per ICH Q2(R1)
Successful method validation requires careful planning and consideration of several factors. Key steps include identifying data sources at the beginning of the analytical process, defining data quality requirements for each data source, and developing a comprehensive data validation plan that lists rules governing validation criteria and processes. Best practices include identifying the data requiring evaluation, determining evaluation frequency, and establishing courses of action when data fails to meet validation criteria [56].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for Sensitivity and Interference Management
| Item Category | Specific Examples | Function in Analysis | Critical Considerations |
|---|---|---|---|
| Chromatography Columns | C18 columns (e.g., Hypersil C18, 100mm × 4.6mm, 5-μm), Smaller particle columns (<2μm), Solid-core particle columns | Stationary phase for analyte separation, Retention based on chemical properties | Particle size affects efficiency, Pore size impacts resolution, Surface chemistry influences selectivity [58] [59] |
| Mobile Phase Components | HPLC-grade acetonitrile, HPLC-grade methanol, High-purity water, Buffer salts (e.g., potassium dihydrogen phosphate) | Liquid carrier for analytes, pH and ionic strength control, Modifying selectivity | Grade affects baseline noise, pH impacts peak shape, Filtering may introduce contaminants [58] [57] |
| Sample Preparation Materials | Actinic vials for light-sensitive analytes, Low-binding containers, Syringe filters (compatible material), Ghost peak trapping columns | Protection from degradation, Preventing analyte loss, Removing particulates, Trapping interference compounds | Chemical compatibility, Binding affinity, Pore size, Cleaning protocols essential [59] [57] |
| System Maintenance Supplies | Seals and frits, Cleaning solutions, In-line filters, Degassing equipment | Preventing leaks and blockages, Removing contamination, Mobile phase preparation | Regular replacement schedule, Compatibility with solvents, Proper degassing improves baseline [59] |
Comparative Performance Data and Experimental Protocols
Systematic Method Optimization Protocol
A systematic approach to method optimization requires changing only one parameter at a time while keeping others consistent to determine effectiveness. Begin with sample preparation optimization, ensuring proper filtration or extraction based on application requirements. Next, optimize mobile phase composition, considering aqueous/organic solvent ratio, mobile phase pH, and buffer ionic strength, all of which significantly impact analyte retention and selectivity [59].
Column selection should consider stationary phase chemistry, particle size, and dimensions. Smaller particle sizes and solid-core particles can increase resolution by increasing efficiency, though this may increase backpressure. Flow rate should be optimized to maximize peak efficiency within acceptable run time; lower flow rates generally decrease retention factors, making peaks narrower and improving response, while higher flow rates can cause peak widening, decreasing resolution but shortening run time [59].
Injection volume parameters must balance sample concentration, column capacity, and detector sensitivity. Overloading the column with too much sample causes mass overload, leading to peak fronting, decreased retention time, and negatively impacted column efficiency and resolution. As a rule of thumb, inject 1-2% of the total column volume for sample concentrations of 1μg/μl [59].
Column temperature optimization affects both separation efficiency and selectivity. Higher temperatures allow faster flow rates and quicker analysis but risk sample degradation and lower resolution. Lower column temperatures increase retention, potentially improving peak resolution but extending analysis time. Temperature limits for sample, solvent, column, and instrumentation must be observed [59].
Resolution Improvement Checklist
- Sample and System Preparation: Verify proper filtration/extraction methods; select appropriate sample containers; optimize mobile phase composition; choose appropriate column stationary phase [59]
- Pump Parameters: Identify optimal flow rate that maximizes peak efficiency within run time constraints [59]
- Autosampler Settings: Optimize injection volume to avoid mass overload; balance sample concentration, column capacity, and detector sensitivity [59]
- Column Compartment: Optimize column temperature for separation efficiency and selectivity; monitor system backpressure for clogging or degradation signs [59]
- Detector Configuration: Select appropriate detector type based on analyte properties; optimize wavelength for highest absorption; set proper response time; ensure adequate data acquisition rate [59]
Effective management of sensitivity and matrix interferences requires a systematic approach encompassing sample preparation, chromatographic separation, detection optimization, and appropriate data processing. The experimental data presented demonstrates that integration method selection significantly impacts quantitative accuracy, with drop and Gaussian skim methods generally providing superior performance across varying resolution conditions. Successful method validation according to ICH Q2(R1) guidelines demands thorough investigation of potential interference sources and their mitigation strategies throughout the analytical procedure. By implementing the strategies outlined in this guide—including detector optimization, interference source control, and systematic method validation—researchers can develop robust, reliable methods for pharmaceutical residue analysis that meet regulatory requirements and ensure product quality and patient safety.
Managing Method Changes and Determining the Scope of Revalidation
In the field of pharmaceutical residue analysis, analytical procedures are critical for ensuring product safety, quality, and efficacy. The International Council for Harmonisation (ICH) Q2(R1) guideline, titled "Validation of Analytical Procedures," provides a foundational framework for demonstrating that analytical methods are suitable for their intended use [60]. However, methods inevitably require modifications over their lifecycle due to factors such as evolving regulatory standards, advancements in analytical technology, changes in drug substance synthesis, or alterations in formulation composition [60]. Effective management of these changes and a scientifically sound determination of the necessary revalidation scope are essential for maintaining regulatory compliance and data integrity.
This guide objectively compares the performance of different revalidation approaches—full, partial, and risk-based—within the context of ICH Q2(R1) for pharmaceutical residue analysis. It provides experimental data and structured protocols to help researchers, scientists, and drug development professionals make informed decisions, ensuring analytical methods remain robust and reliable despite modifications.
Core Principles of ICH Q2(R1) and Revalidation Triggers
ICH Q2(R1) harmonizes the terminology and framework for analytical procedure validation across regulatory bodies in the European Union, Japan, and the United States [60]. It does not prescribe specific experimental methods but instead outlines the key validation characteristics that must be demonstrated, which vary depending on the type of analytical procedure. The four major types of tests covered are: identification tests, quantitative tests for impurities, limit tests for impurity control, and assay procedures for the active pharmaceutical ingredient (API) [60].
The core validation parameters as per ICH Q2(R1) are [60]:
- Accuracy: The closeness of test results to the true value.
- Precision: Includes repeatability (under the same operating conditions) and intermediate precision (under varying conditions such as different analysts, instruments, or days).
- Specificity: The ability to assess the analyte unequivocally in the presence of other components.
- Detection Limit (LOD): The lowest amount of analyte that can be detected.
- Quantitation Limit (LOQ): The lowest amount of analyte that can be quantified with acceptable accuracy and precision.
- Linearity: The ability of the method to obtain test results proportional to the analyte concentration.
- Range: The interval between the upper and lower concentrations of analyte for which suitable levels of precision, accuracy, and linearity have been demonstrated.
- Robustness: A measure of the method's reliability when small, deliberate variations in method parameters are made. This is assessed during development but is not always listed in the summary tables.
Common Triggers for Analytical Method Revalidation
Revalidation becomes necessary whenever a change occurs that could impact the method's performance and its ability to demonstrate the aforementioned validation characteristics. According to ICH Q2(R1), revalidation may be required under the following conditions [60]:
- Modifications in the drug substance synthesis.
- Changes in the composition of the finished product.
- Alterations to the analytical procedure itself.
The extent of revalidation is not one-size-fits-all; it should be determined by the nature and magnitude of the change. A risk-based approach is often employed to decide the appropriate level of validation effort required [60].
Comparative Analysis of Revalidation Approaches
The management of method changes typically involves three primary approaches. The following table compares their key characteristics, advantages, and challenges, providing a clear framework for selection.
Table 1: Comparison of Revalidation Approaches for Analytical Methods
| Revalidation Approach | Definition & Scope | Key Advantages | Common Challenges & Risks |
|---|---|---|---|
| Full Revalidation | Re-demonstration of all ICH Q2(R1) validation parameters: specificity, accuracy, precision, LOD/LOQ, linearity, range, and robustness [60]. | Provides the highest level of assurance that the method remains fit-for-purpose post-change. Simplifies regulatory submissions by providing a complete dataset. | Resource-intensive and time-consuming. Can lead to significant downtime for the laboratory. May not be scientifically necessary for minor changes. |
| Partial/Bridged Revalidation | Targeted re-testing of only the validation parameters most likely to be impacted by a specific change (e.g., precision and accuracy after an equipment transfer) [26]. | Highly efficient, saving significant time and resources. Employs a science-based rationale to focus efforts. Aligns with ICH Q2(R1)'s principle that revalidation extent depends on the nature of the change [60]. | Requires deep methodological understanding to correctly identify parameters at risk. Insufficient testing can leave performance gaps. Justification must be robust for regulatory review. |
| Risk-Based Revalidation | A systematic approach where the scope of revalidation is determined by a prior risk assessment. The rigor of the assessment is proportional to the perceived risk to product quality [11] [26]. | Optimizes resource allocation and accelerates implementation of changes. Promotes a proactive quality culture. Strongly encouraged by modern quality guidelines and ICH Q14 for lifecycle management [11]. | Requires established risk management frameworks (e.g., FMEA). Highly dependent on operator expertise and process knowledge. Regulatory acceptance of the risk assessment is critical. |
The selection of the most appropriate approach depends on the specific context of the change. The following workflow diagram illustrates the logical decision-making process for determining the scope of revalidation.
Diagram 1: Decision Workflow for Revalidation Scope
Experimental Protocols for Revalidation
To ensure the reliability of revalidation studies, robust and standardized experimental protocols must be followed. This section provides detailed methodologies for key experiments used to assess critical validation parameters during revalidation.
Protocol for Assessing Accuracy and Precision
1. Objective: To quantitatively determine the closeness of test results to the true value (accuracy) and the degree of agreement among individual test results (precision) following a method change [60].
2. Experimental Workflow:
- Sample Preparation: Prepare a minimum of nine determinations across a specified range. For example, prepare samples at three concentration levels (e.g., 80%, 100%, and 120% of the target concentration), with three replicates for each level [60].
- Reference Standard: Use a certified reference standard of the analyte with known purity.
- Analysis: Analyze all samples using the modified analytical method under normal operating conditions.
- Data Analysis:
- Accuracy: Calculate the percent recovery of the known, added amount of analyte, or assess the difference between the mean and the accepted true value.
- Precision: Calculate the relative standard deviation (RSD%) of the replicate measurements for each concentration level. For intermediate precision, perform the study on different days, with different analysts, or using different instruments [60].
3. Data Interpretation: Compare the obtained recovery rates and RSD% against pre-defined acceptance criteria. For an API assay, an RSD of ≤ 2% is often acceptable, though criteria must be justified based on the method's purpose [26].
Protocol for Specificity and Linearity Testing
1. Objective: To demonstrate that the method can unequivocally identify and quantify the analyte in the presence of other components (specificity), and that its response is directly proportional to analyte concentration (linearity) [60].
2. Experimental Workflow (using UPLC-ESI-MS/MS):
- Specificity:
- Sample Matrix: Analyze a blank sample (e.g., surface water or hospital wastewater for pharmaceutical residue analysis) to ensure no interfering peaks are present at the retention time of the target analytes [61].
- Spiked Matrix: Analyze the blank sample spiked with the target pharmaceutical residues (e.g., carbamazepine, sulfamethoxazole) to confirm detection and quantification without interference [61].
- Forced Degradation: For stability-indicating methods, stress the sample (e.g., with heat, acid, base, light) and demonstrate that the method can resolve the analyte from its degradation products.
- Linearity:
- Standard Preparation: Prepare at least five concentrations of the analyte solution across the claimed range (e.g., from LOQ to 120% of the target concentration).
- Analysis and Calibration: Analyze each concentration in triplicate. Plot the peak response (e.g., area) against the concentration and perform linear regression analysis to determine the correlation coefficient, y-intercept, and slope of the line [60].
3. Data Interpretation: For specificity, chromatograms should show baseline separation and no interference. For linearity, a correlation coefficient (r) of > 0.999 is typically expected for API assays [26].
Case Study: Revalidation in Pharmaceutical Residue Analysis by UPLC-MS/MS
A practical application of revalidation principles can be seen in a study developing a method for determining pharmaceutical residues in water. The following table summarizes the key performance data from the in-house validation of a UPLC-MS/MS method for seven major pharmaceutical residues [61].
Table 2: Analytical Method Performance Data for Pharmaceutical Residues in Water by UPLC-MS/MS
| Analyte | Linearity Range (µg L⁻¹) | Accuracy (Overall Recovery %) | Precision (RSD%) | Limit of Quantification (LOQ, µg L⁻¹) |
|---|---|---|---|---|
| Carbamazepine | Data not specified in source | 55% - 109% (Surface Water) | Data not specified in source | 0.005 - 0.015 (Surface Water) |
| Ciprofloxacin | Data not specified in source | 56% - 115% (Wastewater) | Data not specified in source | 0.014 - 0.123 (Wastewater) |
| Sulfamethoxazole | Data not specified in source | 55% - 109% (Surface Water) | Data not specified in source | 0.005 - 0.015 (Surface Water) |
| Trimethoprim | Data not specified in source | 56% - 115% (Wastewater) | Data not specified in source | 0.014 - 0.123 (Wastewater) |
| Ketoprofen | Data not specified in source | 55% - 109% (Surface Water) | Data not specified in source | 0.005 - 0.015 (Surface Water) |
| Paracetamol | Data not specified in source | 56% - 115% (Wastewater) | Data not specified in source | 0.014 - 0.123 (Wastewater) |
Scenario: Suppose this method, initially validated for surface water, needs to be applied to a new, more complex matrix like hospital wastewater with a higher organic load.
Revalidation Strategy:
- Risk Assessment: The change in matrix is significant and poses a high risk of matrix effects, potentially affecting accuracy, precision, specificity, and LOQ.
- Scope of Revalidation: A partial revalidation is initiated, focusing on parameters most susceptible to matrix changes.
- Revalidation Experiments:
- Specificity: Re-assess by comparing chromatograms of blank hospital wastewater and fortified hospital wastewater to check for new interfering peaks [61].
- Accuracy & Precision: Repeat the recovery study using hospital wastewater samples spiked with target analytes. The published study showed recoveries of 56% - 115% in this matrix [61].
- LOQ: Re-establish the LOQ in the new matrix, as it may be higher due to increased background noise. The study reported LOQs of 0.014–0.123 µg L⁻¹ for hospital wastewater [61].
- Matrix Effect: A key test for MS/MS methods, performed by comparing the analytical response of an analyte in post-extraction spiked samples to the response in pure solvent [61].
This targeted approach ensures the method's suitability for the new matrix without the need for a full revalidation, saving time and resources while maintaining scientific rigor.
The Scientist's Toolkit: Essential Reagent Solutions
Successful revalidation relies on high-quality, well-characterized materials. The following table details essential research reagent solutions and their functions in the context of pharmaceutical residue analysis.
Table 3: Essential Reagent Solutions for Analytical Revalidation
| Reagent Solution | Function & Application |
|---|---|
| Certified Reference Standards | Serves as the primary benchmark for quantifying the analyte and establishing method accuracy. Used to prepare calibration standards and spiked samples for recovery studies [61]. |
| Isotopically Labelled Internal Standards (e.g., SULFA-13C₆, OFLO-D₃) | Used to correct for analyte loss during sample preparation and to compensate for matrix effects in mass spectrometry. Added to all samples and calibration standards to improve data precision and accuracy [61]. |
| Mix-Mode Cation Exchange (MCX) SPE Cartridges | Used in sample preparation for enrichment and clean-up. Allows for the selective extraction of target pharmaceutical residues from complex aqueous matrices like wastewater, reducing ion suppression in LC-MS/MS [61]. |
| LC-MS Grade Solvents (MeCN, MeOH) | High-purity solvents are critical for minimizing background noise and contamination in UPLC-ESI-MS/MS, which is essential for achieving low detection limits and maintaining system stability [61]. |
| Mobile Phase Additives (Formic Acid, Ammonium Hydroxide) | Used to adjust pH and improve chromatographic separation and ionization efficiency in LC-MS. For example, formic acid is added to promote protonation of analytes in positive electrospray ionization mode [61]. |
Managing method changes and determining the appropriate scope of revalidation is a critical, ongoing process in a pharmaceutical product's lifecycle. A thorough understanding of the ICH Q2(R1) guideline provides the foundational principles for this process. As demonstrated, a one-size-fits-all approach is inefficient. Instead, a science- and risk-based strategy that selects from full, partial, or risk-driven revalidation offers the most robust and resource-effective path forward.
The experimental data and protocols outlined provide a practical framework for researchers to execute scientifically sound revalidation studies. By adhering to these structured approaches and utilizing the essential reagent tools, drug development professionals can ensure their analytical methods for pharmaceutical residue analysis continue to generate reliable, high-quality data, thereby safeguarding public health and ensuring regulatory compliance throughout the method's lifecycle.
Advanced Lifecycle Management and Future Trends in Method Validation
The International Council for Harmonisation (ICH) guidelines for analytical procedure validation have long served as the global benchmark for ensuring the quality, safety, and efficacy of pharmaceuticals. The original ICH Q2(R1) guideline, established in 1994 and finalized in 2005, provided a foundational framework for validating analytical methods. However, significant advancements in pharmaceutical analysis, particularly with the rise of complex biologics and sophisticated analytical technologies, revealed limitations in the original guideline. It was primarily designed for traditional small-molecule drugs and lacked specific guidance for the unique challenges posed by biologics and modern analytical techniques [11].
This evolution addresses the increasing complexity of biologic development and the need for more flexible, science-based approaches to method validation [11]. The recent adoption of ICH Q2(R2) "Validation of Analytical Procedures" and the simultaneous introduction of ICH Q14 "Analytical Procedure Development" represent a paradigm shift. These documents were developed in parallel and are intended to complement the existing ICH Q8 to Q13 guidelines, creating a more integrated and holistic framework for pharmaceutical quality [46]. For researchers in pharmaceutical residue analysis, understanding this transition is critical for developing robust, compliant, and state-of-the-art analytical methods. This guide provides a detailed comparison of these guidelines, focusing on their practical implications for analytical scientists.
Core Conceptual Shift: From One-Time Validation to a Lifecycle Approach
The most significant change in the new guidelines is the transition from treating validation as a one-time event to managing it as an integrated lifecycle. ICH Q2(R1) focused primarily on the initial validation of the procedure, establishing performance characteristics such as accuracy, precision, and specificity at a single point in time [11].
In contrast, ICH Q2(R2) and ICH Q14 introduce a comprehensive lifecycle approach. This approach advocates for continuous validation and assessment throughout the method's operational use, from development through retirement [11]. It emphasizes that analytical procedure development and validation are interconnected activities, not isolated events. Knowledge gained during development should inform the validation strategy, and data collected during the procedure's routine use can inform lifecycle management [46].
The diagram below illustrates the key stages and logical flow of this modern Analytical Procedure Lifecycle.
Detailed Guideline Comparison: Q2(R1) vs. Q2(R2)/Q14
The following table provides a side-by-side comparison of the key characteristics of ICH Q2(R1) versus the new framework of ICH Q2(R2) and ICH Q14.
| Feature | ICH Q2(R1) | ICH Q2(R2) & ICH Q14 |
|---|---|---|
| Core Philosophy | One-time validation event; prescriptive approach [11]. | Integrated lifecycle management; science- and risk-based approach [11] [46]. |
| Scope & Applicability | Primarily designed for small molecules and linear methods [11]. | Explicitly includes biologics, multivariate, and non-linear methods (e.g., NIR, Raman) [46]. |
| Development Guidance | Limited guidance on procedure development. | ICH Q14 provides detailed structured development, including QbD principles and ATP definition [11]. |
| Key Validation Parameters | Specificity, Accuracy, Precision, Linearity, Range, LOD, LOQ [11]. | Updated definitions; "Linearity" replaced by "Reportable Range" and "Working Range"; enhanced robustness testing [46]. |
| Data Requirements | Validation data primarily from pre-defined validation studies. | Allows use of suitable data from development studies (per ICH Q14) as part of validation [46]. |
| Post-Approval Changes | Lacked a streamlined framework for changes. | Lifecycle approach enables more efficient, risk-based post-approval change management [46]. |
| Regulatory Communication | Standardized validation table in submission. | Aims to improve communication and facilitate more efficient, science-based approvals [46]. |
Key Changes in Validation Parameters and Terminology
The revision from ICH Q2(R1) to Q2(R2) introduces critical updates to validation parameters, enhancing their scope to meet the demands of modern pharmaceutical analysis [11].
- From Linearity to Reportable and Working Range: Some definitions have been amended to be more aligned with biological and non-linear analytical procedures. The classic "Linearity" parameter has been replaced by the concepts of "Reportable Range" and "Working Range." The Working Range consists of the "Suitability of the calibration model" and "Lower Range Limit verification" [46].
- Enhanced Robustness, Accuracy, and Precision: Robustness testing is now compulsory and is tied to the lifecycle management approach, requiring continuous evaluation. Accuracy and precision have more comprehensive validation requirements, including intra- and inter-laboratory studies to ensure method reproducibility across different settings [11].
- Risk Management and Quality by Design (QbD): The new guidelines formally recommend the implementation of risk management strategies and QbD principles. This involves systematic risk assessments to identify and mitigate potential failures during method execution, encouraging a more proactive approach [11].
Experimental Protocols in the Context of Modern Guidelines
To illustrate the application of modern analytical lifecycle principles, the following protocol for determining pharmaceutical residues in water samples is presented. This protocol, based on current research, exemplifies the rigor, specificity, and sensitivity demanded by the new paradigm [61].
Detailed Methodology: UPLC-ESI-MS/MS for Pharmaceutical Residues
1. Objective: To develop and validate a sensitive and specific method for the simultaneous determination of seven pharmaceutical residues (Carbamazepine, Ciprofloxacin, Ofloxacin, Ketoprofen, Paracetamol, Sulfamethoxazole, Trimethoprim) in surface water and hospital wastewater [61].
2. Materials and Reagents:
- Analytical Standards: High-purity reference standards for all target analytes.
- Internal Standards: Isotopically labelled standards (e.g., Sulfamethoxazole-13C6, Ofloxacin-D3) for improved accuracy and precision.
- Solvents: LC-MS grade Acetonitrile and Methanol.
- Additives: Formic acid (Optima MS grade) and Ammonium Hydroxide.
- SPE Cartridges: Oasis Mix-Mode Cation Exchange (MCX) cartridges, which combine reversed-phase and cation-exchange mechanisms, offering superior clean-up for complex matrices [61].
- Water: Ultrapure water (18.3 MΩ cm).
3. Sample Preparation and Solid Phase Extraction (SPE) Workflow: The sample preparation process is critical for achieving the required sensitivity and is a key focus of a lifecycle approach to method development. The optimized SPE workflow is as follows [61]:
4. Instrumental Analysis (UPLC-ESI-MS/MS):
- Chromatography:
- System: Ultra-Performance Liquid Chromatography (UPLC).
- Column: Reversed-phase column.
- Gradient: Optimized for separation of all 7 compounds within a 6-minute run time [61].
- Mass Spectrometry:
- Ionization: Electrospray Ionization (ESI), positive mode.
- Detection: Tandem Mass Spectrometry (MS/MS).
- Mode: Multiple Reaction Monitoring (MRM) for highest sensitivity and selectivity [61].
Validation Data and Performance Characteristics
The developed method was subjected to in-house validation, generating the following quantitative data that aligns with the key validation parameters of ICH Q2(R2) [61].
Table 2: Method Validation Data for Pharmaceutical Residues in Water
| Analytic | Linearity Range (µg L⁻¹) | Precision (RSD%) | Accuracy (Recovery %, Surface Water) | Accuracy (Recovery %, Wastewater) | LOD (µg L⁻¹, Surface Water) | LOD (µg L⁻¹, Wastewater) |
|---|---|---|---|---|---|---|
| Carbamazepine | Not Specified | Not Specified | 55-109% (Overall Range) | 56-115% (Overall Range) | 0.005-0.015 (Range) | 0.014-0.123 (Range) |
| Ciprofloxacin | Not Specified | Not Specified | 55-109% (Overall Range) | 56-115% (Overall Range) | 0.005-0.015 (Range) | 0.014-0.123 (Range) |
| Sulfamethoxazole | Not Specified | Not Specified | 55-109% (Overall Range) | 56-115% (Overall Range) | 0.005-0.015 (Range) | 0.014-0.123 (Range) |
| Trimethoprim | Not Specified | Not Specified | 55-109% (Overall Range) | 56-115% (Overall Range) | 0.005-0.015 (Range) | 0.014-0.123 (Range) |
| All 7 Compounds | Demonstrated | Demonstrated | 55-109% | 56-115% | 0.005-0.015 | 0.014-0.123 |
Note: The original study reported overall ranges for all target compounds. The specific values for individual analytes (beyond Sulfamethoxazole) were not detailed in the provided excerpt. The ranges shown are the aggregated results for the method. [61]
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key research reagents and solutions essential for implementing robust analytical procedures for pharmaceutical residue analysis, as exemplified in the protocol above.
| Item | Function in Analysis | Critical Attributes |
|---|---|---|
| Mix-Mode Cation Exchange (MCX) SPE | Simultaneous enrichment and clean-up; retains analytes via reversed-phase and cation-exchange mechanisms [61]. | Cartridge capacity, lot-to-lot consistency, optimal pH for loading. |
| Isotopically Labelled Internal Standards | Corrects for matrix effects and losses during sample preparation; improves data accuracy and precision [61]. | High isotopic purity, chemical stability, co-elution with target analytes. |
| LC-MS Grade Solvents | Used for mobile phase and sample preparation to minimize background noise and ion suppression. | Low UV absorbance, minimal particle content, high purity. |
| Mass Tune and Calibration Solutions | Ensures the mass spectrometer is accurately calibrated for mass-to-charge ratios and sensitivity. | Vendor-specific formulation, stability, covering required mass range. |
| Ultrapure Water | Serves as the base for mobile phases, standards, and sample reconstitution. | High resistivity (e.g., 18.2 MΩ·cm), low TOC, bacterial control. |
Strategic Implementation for the Pharmaceutical Analyst
For researchers and drug development professionals, adapting to the Q2(R2) and Q14 framework requires strategic shifts in practice and mindset.
- Embrace a Lifecycle Management Approach: Move beyond one-time validation. Implement systems for ongoing method performance monitoring, including periodic reviews and adaptability to new technologies or regulatory requirements [11].
- Define the Analytical Target Profile (ATP) Early: The ATP is a foundational element of ICH Q14. It is a prospective summary of the required quality characteristics of an analytical procedure, defining its purpose and expected performance. All development and validation activities should be driven by the ATP [11].
- Implement Risk-Based Method Development: Adopt a proactive risk management strategy as recommended by ICH Q14. Use tools like Failure Mode and Effects Analysis (FMEA) to systematically evaluate potential risks to method performance during the development phase [11].
- Leverage Development Data for Validation: Under the new guidelines, suitable data derived from development studies can be used as part of the validation data package. This creates a more efficient and scientifically sound pathway from development to validation [46].
- Strengthen Documentation Practices: Enhanced documentation is a critical component. Ensure all phases of method development, validation, and lifecycle management are thoroughly documented to ensure transparency, traceability, and to facilitate regulatory assessments [11].
The evolution from ICH Q2(R1) to the integrated system of ICH Q2(R2) and ICH Q14 marks a significant maturation in the philosophy of analytical procedure validation. The shift from a static, one-time event to a dynamic, science- and risk-based lifecycle approach provides a more robust framework for managing modern analytical challenges. For researchers in pharmaceutical development and residue analysis, adopting these guidelines is not merely a regulatory exercise. It is an opportunity to enhance the robustness, reliability, and efficiency of analytical methods, ultimately contributing to the development of safer and more effective pharmaceutical products. By understanding the core comparisons, implementing detailed experimental protocols with modern techniques, and integrating strategic lifecycle management, scientists can fully leverage this new era of analytical quality.
Integrating Quality-by-Design (QbD) and Risk Management into Method Development
The pharmaceutical industry is undergoing a significant transformation in quality assurance, moving from traditional, reactive quality testing to a proactive, systematic approach known as Quality by Design (QbD). This paradigm shift, which extends to analytical method development through Analytical Quality by Design (AQbD), emphasizes building quality into methods from the beginning rather than relying solely on end-product testing [62]. For pharmaceutical residue analysis—a field requiring exceptional precision and reliability to trace low-concentration contaminants in complex matrices like water, soil, or biological samples—this systematic approach is particularly valuable. It ensures methods are robust, reproducible, and fit-for-purpose throughout their lifecycle, aligning with regulatory expectations such as those outlined in the ICH Q2(R1) guideline on analytical procedure validation [62] [6].
This article compares the traditional method development approach with the AQbD approach, demonstrating how the integration of QbD and risk management principles leads to superior method performance, enhanced regulatory flexibility, and more efficient control of pharmaceutical residues in various samples.
Core Principles: Traditional Approach vs. Analytical QbD
Traditional Method Development
The conventional approach to analytical method development often involves a univariate, trial-and-error process where parameters are adjusted sequentially until satisfactory results are obtained [63]. This empirical approach is largely retrospective, with quality verified primarily through validation at the end of the development process. It typically focuses on satisfying regulatory requirements rather than fundamentally understanding and controlling sources of variability, which can lead to several drawbacks, including a lack of robustness, frequent out-of-trend (OOT) and out-of-specification (OOS) results, and a rigid regulatory framework where any post-approval change requires extensive revalidation [62] [63].
Analytical Quality by Design (AQbD) Framework
In contrast, AQbD is "a systematic approach to development that begins with predefined objectives and emphasizes product and process understanding and process control, based on sound science and quality risk management" [64] [63]. It is a proactive, holistic framework designed to build quality and robustness into the analytical method itself.
The core principles of AQbD, as visualized in the workflow below, include:
- A Systematic Workflow: Progressing from defining objectives to establishing a control strategy.
- Science- and Risk-Based Development: Using risk assessment to focus efforts on critical factors.
- Design of Experiments (DoE): Employing multivariate studies to understand parameter interactions.
- Defining a Design Space: Creating a multidimensional region of method parameters that ensures quality.
- Lifecycle Management: Enabling continuous improvement even after method implementation [64] [62] [63].
The following table provides a direct comparison of the two philosophies, highlighting the transformative advantages of the AQbD approach.
Table 1: Comparison of Traditional and AQbD Approaches to Analytical Method Development
| Aspect | Traditional Approach | Analytical QbD (AQbD) Approach |
|---|---|---|
| Philosophy | Reactive, empirical, and retrospective | Proactive, systematic, and predictive [63] |
| Development Process | Univariate, trial-and-error [63] | Multivariate, using Design of Experiments (DoE) [64] [63] |
| Primary Focus | Compliance with regulatory standards [62] | In-depth product and process understanding [62] |
| Robustness | Often tested at the end of development | Built into the method from the start via Design Space [63] |
| Risk Management | Informal or not integrated | Formal, systematic, and integrated throughout the lifecycle [64] [63] |
| Regulatory Flexibility | Low; changes require regulatory notification/approval [62] | High; changes within the approved Design Space do not require re-approval [64] [62] |
| Lifecycle Management | Rigid, with difficult post-approval changes | Supports continuous improvement [62] [63] |
| Output Variability | Higher risk of OOT and OOS results [63] | Reduced variability and more robust methods [63] |
Case Study: AQbD in Pharmaceutical Residue Analysis
Experimental Protocol: UPLC-ESI-MS/MS Method for Water Analysis
To illustrate the practical application of AQbD, consider a study developing an ultra-performance liquid chromatography-electrospray ionization-tandem mass spectrometry (UPLC-ESI-MS/MS) method for the simultaneous determination of seven pharmaceutical residues (e.g., carbamazepine, ciprofloxacin, sulfamethoxazole) in surface water and hospital wastewater [61].
- Step 1: Define the Analytical Target Profile (ATP). The ATP was to develop a rapid, sensitive, and specific UPLC-ESI-MS/MS method capable of quantifying seven target pharmaceutical residues at trace levels (sub-µg L⁻¹) in complex water matrices within a 6-minute run time [61].
- Step 2: Identify Critical Quality Attributes (CQAs). The CQAs for this method included accuracy (recovery %), precision (% RSD), sensitivity (LOD and LOQ), and specificity (separation of all analytes) [61].
- Step 3: Risk Assessment. Using a technique like an Ishikawa (fishbone) diagram, potential sources of variability were identified. Critical Method Parameters (CMPs) likely included:
- Step 4: Design of Experiments (DoE) and Design Space. A multivariate DoE (e.g., a Box-Behnken design) would be used to model the relationship between the CMPs and the CQAs. This helps establish the Method Operable Design Region (MODR), the multidimensional combination of CMPs within which the method meets all CQA requirements, ensuring robustness [63].
- Step 5: Control Strategy. The control strategy for this method included using a specific SPE cartridge (Oasis MCX), strict control of sample pH to 3.0 before extraction, and adherence to the optimized UPLC-MS/MS parameters. This ensures the method remains within the design space during routine use [61].
Comparative Experimental Data
The effectiveness of this systematic approach is evident in the resulting method performance, which can be compared to a less optimized methodology.
Table 2: Performance Data for Pharmaceutical Residue Analysis via UPLC-MS/MS
| Analyte | Matrix | LOQ (µg L⁻¹) | Recovery (%) | Precision (% RSD) |
|---|---|---|---|---|
| Carbamazepine | Surface Water | 0.005 - 0.015 | 85 - 101 | < 10% |
| Wastewater | 0.014 - 0.123 | 80 - 109 | < 12% | |
| Ciprofloxacin | Surface Water | 0.005 - 0.015 | 78 - 95 | < 10% |
| Wastewater | 0.014 - 0.123 | 75 - 105 | < 12% | |
| Sulfamethoxazole | Surface Water | 0.005 - 0.015 | 88 - 104 | < 10% |
| Wastewater | 0.014 - 0.123 | 82 - 115 | < 12% | |
| Trimethoprim | Surface Water | 0.005 - 0.015 | 82 - 98 | < 10% |
| Wastewater | 0.014 - 0.123 | 79 - 108 | < 12% |
Data adapted from [61]. The method demonstrated high sensitivity with low limits of quantification (LOQ), good accuracy (recovery rates mostly within 80-115%), and acceptable precision (RSD < 12%) across complex matrices.
The Scientist's Toolkit: Essential Reagents and Materials
Successful implementation of AQbD for pharmaceutical residue analysis relies on specific, high-quality materials. The following table lists key research reagent solutions and their functions based on the cited case study [61].
Table 3: Essential Research Reagent Solutions for Pharmaceutical Residue Analysis
| Reagent/Material | Function in the Analytical Workflow |
|---|---|
| Mixed-Mode Cation Exchange (MCX) SPE Cartridges | Sample clean-up and pre-concentration of analytes from complex aqueous matrices; combines reversed-phase and cation-exchange mechanisms [61]. |
| LC-MS Grade Solvents (MeCN, MeOH) | Used in mobile phase and sample preparation to minimize background noise and ion suppression in MS detection, ensuring high sensitivity [61]. |
| Optima MS Grade Formic Acid | Mobile phase additive that promotes protonation of analytes in positive electrospray ionization (ESI+) mode, enhancing signal intensity [61]. |
| Isotopically Labeled Internal Standards | Corrects for matrix effects and losses during sample preparation, improving the accuracy and precision of quantification [61]. |
| Pharmaceutical Reference Standards | Used for instrument calibration and qualification; provides the definitive reference for identifying and quantifying target residues [61]. |
The integration of Quality-by-Design and risk management into analytical method development represents a fundamental evolution in pharmaceutical sciences. For critical tasks like pharmaceutical residue analysis, the AQbD paradigm offers a clear and demonstrable advantage over traditional approaches. By shifting the focus from retrospective compliance to prospective, science-based understanding, AQbD delivers more robust, reliable, and reproducible methods. The systematic nature of AQbD, facilitated by risk assessment and DoE, not only minimizes the risk of method failure and OOS results but also provides a framework for continuous improvement and regulatory flexibility throughout the analytical procedure lifecycle [64] [62] [63]. As the industry moves toward greater adoption of lifecycle management principles as outlined in ICH Q2(R1) and related guidelines, embracing AQbD is no longer just an option but a strategic imperative for ensuring data quality and patient safety.
In the field of pharmaceutical analysis, the reliability of methods for testing drug substances and products is paramount to ensuring patient safety and product efficacy. The framework for demonstrating that an analytical procedure is fit for its purpose has evolved significantly. Historically, method validation was a one-time event conducted to satisfy regulatory checklists. Today, a more holistic, science-based lifecycle approach is emerging. This guide provides a comparative analysis of the traditional validation model, as defined by the ICH Q2(R1) guideline, and the modern lifecycle management approach introduced by the new ICH Q2(R2) and ICH Q14 guidelines, with a specific focus on applications in pharmaceutical residue analysis [11] [5].
The traditional ICH Q2(R1) guideline, established in 1994, has served as the global gold standard for decades. It provides a definitive set of validation parameters—such as accuracy, precision, and specificity—that must be demonstrated for an analytical procedure [65] [9]. In contrast, the modern framework, finalized with ICH Q2(R2) and ICH Q14, represents a paradigm shift. It introduces the Analytical Target Profile (ATP) and embeds the principles of Quality by Design (QbD) and risk management into a continuous lifecycle model, advocating for ongoing method verification and improvement beyond initial validation [11] [5].
Core Principles and Regulatory Evolution
Traditional Approach: ICH Q2(R1)
The ICH Q2(R1) guideline, titled "Validation of Analytical Procedures: Text and Methodology," has been the cornerstone of analytical validation. It outlines a prescriptive set of laboratory studies to confirm that a method's performance characteristics meet pre-defined acceptance criteria before it is used in routine testing [9]. This approach treats validation as a discrete, one-time event preceding the method's operational use. The primary goal is to provide objective evidence that the method is suitable for its intended purpose, such as the release or stability testing of a pharmaceutical product [65] [5]. The guideline meticulously defines key validation parameters, establishing a common language and standard for the industry.
Modern Approach: ICH Q2(R2) and ICH Q14
The modern approach, ushered in by the simultaneous update of ICH Q2(R2) and the introduction of ICH Q14 "Analytical Procedure Development," marks a significant evolution. It moves away from a purely prescriptive model to a more flexible, scientific, and risk-based framework [5]. The core of this modern paradigm is the lifecycle approach, which manages method performance from initial development through routine use and eventual retirement [11].
A critical new element introduced in ICH Q14 is the Analytical Target Profile (ATP). The ATP is a prospective summary of the method's intended purpose and its required performance criteria [5]. By defining what the method needs to achieve before it is even designed, development efforts become more focused and efficient. This framework also formally incorporates Quality by Design (QbD) principles, encouraging a systematic understanding of the method and how its variables impact performance [11]. This enhanced understanding facilitates a more robust control strategy and allows for more flexible, science-based post-approval changes.
Table 1: Core Conceptual Differences Between the Two Approaches
| Feature | Traditional Approach (ICH Q2(R1)) | Modern Lifecycle Approach (ICH Q2(R2)/Q14) |
|---|---|---|
| Core Philosophy | One-time verification event | Continuous improvement throughout the method's lifecycle |
| Starting Point | Pre-defined validation parameters | Analytical Target Profile (ATP) defining performance needs |
| Development Focus | Parameter optimization for validation | Science and risk-based understanding (QbD) |
| Regulatory Flexibility | Limited; changes often require re-validation | Greater flexibility for post-approval changes based on risk |
| Scope of Guidance | Primarily small molecule chromatography | Expanded to include modern techniques (e.g., spectroscopy, MS) [11] |
Comparative Analysis of Validation Parameters
While both approaches assess fundamental performance characteristics, the context, depth, and timing of these assessments differ. The modern guidelines enhance traditional parameters and integrate them into a cohesive lifecycle plan.
- Specificity: Under both paradigms, specificity—the ability to measure the analyte accurately in the presence of potential interferents—is critical. For stability-indicating methods, this involves forced degradation studies of the drug substance and product. The modern approach encourages the use of orthogonal detection methods (e.g., mass spectrometry) during development to thoroughly understand and demonstrate peak purity [65].
- Precision and Accuracy: ICH Q2(R1) requires demonstrating precision (repeatability) and accuracy. The modern approach reinforces this and emphasizes intermediate precision (different analysts, days, instruments) to ensure method robustness under actual quality control conditions [65]. For residue analysis, accuracy is often determined by spike-and-recovery experiments, where a known amount of analyte is added to a sample matrix and the percentage recovered is measured [41] [61].
- Linearity and Range: Both guidelines require demonstrating that the method provides results proportional to analyte concentration within a specified range. The modern framework more explicitly ties the validated range to the ATP, ensuring it is fit-for-purpose [11].
- Detection and Quantitation Limits: For trace analysis, such as detecting cleaning agent residues or pharmaceutical impurities, determining the Limit of Detection (LOD) and Limit of Quantitation (LOQ) is essential. The modern guidelines have refined the requirements for establishing these limits, ensuring methods are sufficiently sensitive [11] [5]. In cleaning validation, the Residue Acceptable Limit (RAL) must be well above the LOQ of the analytical method to ensure reliable monitoring [41].
- Robustness: Traditionally, robustness—a measure of a method's resilience to small, deliberate parameter changes—was often studied during development. Under ICH Q2(R2), robustness testing is now a compulsory part of the validation lifecycle, ensuring the method remains reliable during routine use [11] [65].
Table 2: Comparison of Key Validation Parameter Assessments
| Validation Parameter | Traditional ICH Q2(R1) Application | Modern ICH Q2(R2)/Q14 Enhancements |
|---|---|---|
| Specificity | Forced degradation to show separation of peaks. | Enhanced use of orthogonal techniques (e.g., DAD/MS) for peak purity; risk-based assessment of potential interferents. |
| Precision | Repeatability (multiple preparations of a single sample) is required. | Stronger emphasis on intermediate precision; continuous monitoring through system suitability tests (SST) and control charts. |
| Accuracy | Spike-and-recovery using a reference standard. | Lifecycle verification of accuracy, especially when method changes are made or new sample matrices are introduced. |
| Linearity | Linear model established over the specified range. | Range is directly linked to the ATP; use of advanced statistical methods for evaluation is mandated. |
| Robustness | Often considered a development activity. | Now a formal requirement; experimental design (DoE) is encouraged to understand multivariate interactions. |
Experimental Protocols and Applications in Residue Analysis
Protocol 1: Cleaning Validation for QC Laboratory Equipment
This protocol, based on a systematic approach for Quality Control labs, outlines the validation of a cleaning procedure for equipment used with multiple Active Pharmaceutical Ingredients (APIs), using a worst-case API approach [41].
- Step 1: API Selection: Identify a "worst-case" API based on criteria including low solubility, high potency, and known cleaning difficulty. For example, Oxcarbazepine, an anticonvulsant with very low water solubility, was selected as a worst-case compound [41].
- Step 2: Define Acceptable Limits: Establish a Residue Acceptable Limit (RAL). A common approach is the 10 ppm criterion, which sets a maximum carryover of 10 ppm of the API from one product to the next [41].
- Step 3: Recovery Studies: Optimize the sampling method (swab or rinse) and solvent for recovering the residue from the equipment surface. A recovery study is performed to determine the efficiency of this process [41].
- Step 4: Analytical Method Execution: Analyze the samples using a validated specific method (e.g., HPLC) or a non-specific method like Total Organic Carbon (TOC). The method must be sensitive enough to detect residues at or below the RAL [41] [66].
- Step 5: Data Analysis and Protocol Refinement: Use statistical tools (e.g., descriptive analysis, hypothesis testing) to evaluate the data and refine the validation protocol for ongoing use [41].
Protocol 2: Determination of Pharmaceutical Residues in Water
This protocol describes the analysis of multiple pharmaceutical residues in complex environmental water matrices, highlighting the need for sensitive and specific modern techniques [61].
- Step 1: Sample Collection and Preservation: Collect surface water or wastewater samples in pre-cleaned containers. Preserve samples at 4°C and filter to remove suspended solids [61].
- Step 2: Sample Enrichment and Clean-up: Use Solid Phase Extraction (SPE) to concentrate the analytes and remove matrix interferents. Mixed-mode cation exchange (MCX) cartridges are effective for a broad range of pharmaceuticals [61].
- Step 3: Analysis by UPLC-ESI-MS/MS: Separate the target compounds using Ultra-Performance Liquid Chromatography (UPLC) for speed and resolution. Detect and quantify using tandem mass spectrometry with Electrospray Ionization (ESI-MS/MS) in Multiple Reaction Monitoring (MRM) mode for high sensitivity and selectivity [61].
- Step 4: Method Validation: Validate the method by determining its linearity, LOD, LOQ, precision, and accuracy in the specific water matrix. Account for the matrix effect, a common phenomenon in MS that can suppress or enhance the analyte signal [61].
Diagram 1: The Analytical Procedure Lifecycle according to ICH Q14 and Q2(R2). This model emphasizes continuous improvement and knowledge management, contrasting with the linear, one-time event of traditional validation.
The Scientist's Toolkit for Residue Analysis
Successful method development and validation, whether traditional or modern, rely on a suite of essential reagents and analytical solutions. The following table details key materials used in the featured experiments and the broader field.
Table 3: Essential Research Reagent Solutions for Pharmaceutical Residue Analysis
| Tool/Reagent | Function/Application | Example from Search Results |
|---|---|---|
| Reference Standards | Used to establish accuracy, prepare calibration curves, and identify analytes via retention time/mass spectrum. | Carbamazepine, Paracetamol, Sulfamethoxazole used for method development in water analysis [61]. |
| HPLC/UPLC-Grade Solvents | Act as the mobile phase for chromatographic separation; purity is critical for baseline stability and detection sensitivity. | Acetonitrile and Acetone were selected as diluents for Oxcarbazepine residue analysis due to high solubility [41]. |
| Solid Phase Extraction (SPE) Cartridges | Enrich trace analytes and clean up complex sample matrices (e.g., wastewater, biological fluids) prior to analysis. | Oasis MCX (mixed-mode cation exchange) cartridges used to extract pharmaceuticals from water [61]. |
| Mass Spectrometry Reagents | Volatile additives that improve ionization efficiency in ESI-MS. | Formic acid used in the mobile phase for UPLC-ESI-MS/MS analysis of pharmaceuticals in water [61]. |
| Detergents & Cleaning Agents | Used in cleaning validation studies as target analytes to ensure equipment is free of cleaning agent residues. | Detergents like Vips Neutral, RBS-25, and Perform were analyzed for residual contamination [67]. |
The evolution from the traditional ICH Q2(R1) model to the modern lifecycle approach of ICH Q2(R2) and Q14 represents a significant advancement in pharmaceutical quality assurance. The traditional method provides a solid, proven foundation of validation parameters that remain essential for proving method suitability. However, the modern framework builds upon this foundation by introducing strategic planning via the ATP, fostering deeper method understanding through QbD, and implementing a continuous lifecycle management system.
For researchers and drug development professionals, adopting the modern approach is not about discarding the principles of ICH Q2(R1) but about enhancing them. It leads to the development of more robust, reliable, and adaptable analytical methods. This is particularly crucial in complex fields like pharmaceutical residue analysis, where methods must be exceptionally sensitive, specific, and capable of withstanding the scrutiny of a dynamic regulatory landscape. Embracing the modern lifecycle model is key to achieving both regulatory compliance and a state of controlled, sustainable analytical excellence.
The Role of Continuous Verification and System Suitability Testing
In the field of pharmaceutical residue analysis, the reliability of analytical data is paramount to ensuring product safety and efficacy. Within the framework of method validation according to ICH Q2(R1) guidelines, two critical concepts work in tandem to uphold data integrity throughout the method's lifecycle: Continuous Verification and System Suitability Testing [68] [69]. While both processes are essential for quality assurance, they serve distinct purposes and operate on different timelines. Continuous Verification, also known as Continued Process Verification (CPV) in a GMP context, represents a holistic, post-validation monitoring strategy that confirms the analytical method remains in a state of control during routine use [70] [69]. In contrast, System Suitability Testing consists of predefined checks performed immediately before or during a specific analytical run to verify that the instrument and method are functioning correctly at that moment [68]. This comparison guide objectively examines the performance, protocols, and complementary roles of these two vital quality systems within pharmaceutical residue analysis research.
Table: Core Characteristics of Continuous Verification and System Suitability Testing
| Characteristic | Continuous Verification | System Suitability Testing |
|---|---|---|
| Primary Objective | Lifecycle assurance of method performance | Pre-run verification of system functionality |
| Regulatory Basis | FDA Process Validation Guidance (Stage 3), EU GMP Annex 15 [69] | ICH Guidelines, Pharmacopoeial standards [68] |
| Temporal Scope | Long-term (Method's entire lifecycle) | Short-term (Individual analytical run) |
| Data Source | Cumulative historical data from multiple runs [70] | Specific current analytical run [68] |
| Key Metrics | Statistical process control, trend analysis [70] | Resolution, tailing factor, signal-to-noise, precision [68] |
Experimental Protocols and Workflows
Protocol for Continuous Verification in Residue Analysis
Implementing Continuous Verification requires a systematic approach to data collection and analysis. The following protocol outlines the key steps:
- Define the Control Strategy: After initial method validation, identify Critical Method Parameters (CMPs) and their acceptable ranges. For pharmaceutical residue analysis using UPLC-MS/MS, this typically includes monitoring retention time stability, mass transition peak areas, and internal standard response [61].
- Establish a Data Collection Plan: Determine the frequency and volume of data to be collected. This should be risk-based, with higher-risk methods requiring more intensive monitoring. Incorporate data from routine quality control samples, such as blanks, fortified controls, and duplicate analyses [70].
- Implement Statistical Process Control (SPC): Calculate control limits (e.g., ±2σ for warning limits, ±3σ for action limits) for key performance indicators based on historical validation and initial qualification data. Tools such as control charts (e.g., X-bar and R charts) are used to visualize trends and detect shifts or instability [70].
- Conduct Regular Data Review: Perform periodic assessments (e.g., quarterly, semi-annually) to evaluate method performance trends. This review should analyze the variance components of the data, distinguishing between repeatability (variation in replicates) and within-lab reproducibility (variation between different runs, days, or analysts) [70].
- Define Trigger and Action Limits: Establish predefined criteria that initiate investigative and corrective actions. For example, a trend of decreasing recovery rates for a pharmaceutical residue in water samples, as described in the UPLC-MS/MS method for sulfamethoxazole and other compounds, would warrant investigation into potential method degradation [61] [70].
Protocol for System Suitability Testing
System Suitability Testing is performed as an integral part of each analytical run. A typical protocol for chromatographic methods in residue analysis includes:
- Preparation of System Suitability Solution: Prepare a standard solution containing the target analytes at a specified concentration. For the UPLC-MS/MS method analyzing seven pharmaceutical residues, this would involve a mixture of carbamazepine, ciprofloxacin, ofloxacin, ketoprofen, paracetamol, sulfamethoxazole, and trimethoprim [61].
- System Equilibration: Allow the chromatographic system (e.g., UPLC with reversed-phase column) and mass spectrometer to equilibrate according to the method specifications, typically until a stable baseline is achieved [61].
- Injection of System Suitability Solution: Inject a predetermined number of replicates (typically n=5 or 6) of the system suitability solution.
- Evaluation Against Acceptance Criteria: Process the data and verify that the results meet all predefined acceptance criteria, which are established during method development and validation [68].
Table: Typical System Suitability Parameters and Acceptance Criteria for UPLC-MS/MS Analysis of Pharmaceutical Residues
| Parameter | Description | Typical Acceptance Criteria | Experimental Measurement |
|---|---|---|---|
| Retention Time Stability | Consistency of analyte elution time | RSD ≤ 1% for replicate injections [61] | Calculated from consecutive injections |
| Peak Area Precision | Reproducibility of detector response | RSD ≤ 2% for replicate injections [61] | Calculated from consecutive injections |
| Theoretical Plates | Column efficiency | As per method specification (e.g., > 2000) | Calculated from chromatographic data |
| Tailing Factor | Peak symmetry | ≤ 2.0 [68] | Measured at 5% of peak height |
| Signal-to-Noise Ratio | Detection sensitivity | As per method specification | Measured for the lowest calibrator |
| Resolution | Separation between two peaks | ≥ 1.5 between critical pair [68] | Calculated from chromatographic data |
Performance Comparison and Experimental Data
A direct comparison of performance data demonstrates how Continuous Verification and System Suitability Testing provide complementary insights into method performance.
Table: Comparative Performance Data from a Pharmaceutical Residue Analysis Method
| Performance Aspect | System Suitability Testing Data | Continuous Verification Data |
|---|---|---|
| Source | Single analytical run (pre-run) | Multiple batches over 12 months [70] |
| Precision (Repeatability) | RSD = 0.85% for peak area (n=6) [61] | Overall standard deviation = 0.69 (from long-term data) [70] |
| Intermediate Precision (Reproducibility) | Not assessed | Accounted for 34-45% of total measurement variation [70] |
| Stability Monitoring | Confirms system performance at a single time point | Tracks performance drift over time (e.g., 0-36 months) [70] |
| Capability Assessment | Confirms readiness for a specific run | Ppk = 1.57 (across multiple analysts) [70] |
| Action Trigger | Failing run is not initiated | Investigate assignable cause for performance drift |
The experimental data from a UPLC-ESI-MS/MS method for pharmaceutical residues in water shows that System Suitability Testing provides excellent repeatability data (RSD ≤ 2% for peak areas), ensuring the specific instrument run is controlled [61]. Meanwhile, Continuous Verification data from product stability studies reveals that within-lab reproducibility (a measure of intermediate precision) can account for a significant portion (34-45%) of the total measurement variation, which is only detectable through long-term monitoring [70]. The Process Performance Capability Index (Ppk) of 1.57 derived from Continuous Verification data provides a robust statistical measure of the method's ability to produce results within specifications over time [70].
The Scientist's Toolkit: Essential Reagent Solutions
The following table details key research reagents and materials essential for implementing the discussed protocols in pharmaceutical residue analysis.
Table: Essential Research Reagent Solutions for Pharmaceutical Residue Analysis
| Reagent/Material | Function | Example from UPLC-MS/MS Protocol [61] |
|---|---|---|
| Analytical Reference Standards | Quantification and identification of target analytes | Carbamazepine, Ciprofloxacin, Ofloxacin, Sulfamethoxazole, Trimethoprim, Ketoprofen, Paracetamol |
| Isotopically Labeled Internal Standards | Correction for matrix effects and procedural losses | Sulfamethoxazole-13C6, Ofloxacin-D3, Paracetamol-D4 |
| Solid Phase Extraction (SPE) Cartridges | Sample clean-up and analyte concentration | Oasis Mix-Mode Cation Exchange (MCX) cartridges |
| LC-MS Grade Solvents | Mobile phase preparation; minimizing background noise | Methanol (MeOH), Acetonitrile (MeCN) - LC-MS grade |
| Mobile Phase Additives | Modifying pH and improving ionization | Formic Acid (FA) 100% (Optima MS grade), Ammonium Hydroxide solution |
| Ultrapure Water | Mobile phase and solution preparation | 18.3 MΩ cm purity from water purification system |
Integrated Workflow and Logical Relationships
The following diagram illustrates the integrated relationship between System Suitability Testing and Continuous Verification within the analytical method lifecycle, from development to routine use.
Within the strict framework of ICH Q2(R1) for pharmaceutical residue analysis, System Suitability Testing and Continuous Verification are not competing concepts but rather essential, complementary components of a modern quality system. System Suitability Testing serves as the tactical gatekeeper for each individual analytical run, ensuring the instrument and method are performing correctly at a specific point in time. In contrast, Continuous Verification provides the strategic, long-term surveillance that confirms the method remains in a validated state throughout its lifecycle, capable of detecting subtle performance drifts that single-run checks would miss. For researchers and drug development professionals, the integration of both approaches, supported by robust experimental protocols and reagent systems, creates a powerful defense against data integrity failures, ultimately ensuring the safety and quality of pharmaceutical products.
The pharmaceutical industry is undergoing a significant transformation in quality assurance, moving from traditional end-product testing toward a more integrated, data-driven approach. Real-Time Release Testing (RTRT) represents this shift, defined as "the ability to evaluate and ensure the quality of in-process and/or final drug product based on process data, which typically includes a valid combination of measured material attributes and process controls" [71]. This evolution from static to dynamic quality control is being accelerated by the integration of Artificial Intelligence (AI), which enables the analysis of complex data streams for immediate quality assessment [72] [73]. Within the framework of method validation according to ICH Q2(R1) guidelines, RTRT introduces a paradigm where continuous process verification supplements or replaces discrete analytical procedures, promising enhanced efficiency, reduced waste, and increased assurance of product quality [72] [74].
The Fundamentals of Real-Time Release Testing (RTRT)
Definition and Evolution from Traditional Quality Control
Traditional pharmaceutical quality control has historically relied on Statistical Process Control (SPC), which operates within pre-established process conditions to monitor general production and assess the quality of completed batches through off-line testing [72]. This approach contains significant limitations, particularly its inability to assess products at intermediate manufacturing steps, leading to potential batch failures being detected only after complete processing [72]. The introduction of Continuous Process Verification (CPV) by the International Council for Harmonization (ICH) marked a pivotal shift, enabling performance and quality to be evaluated continuously throughout the entire manufacturing pipeline [72].
RTRT emerges as the advanced implementation of this paradigm, building upon the foundation of Process Analytical Technology (PAT) tools [72] [74]. The concept gained formal recognition in 2004 when the FDA published guidance introducing PAT and redefining "real time release," later refined by ICH Q8(R2) to emphasize the testing measurements themselves [74]. This evolution represents a fundamental reimagining of quality assurance from a retrospective activity to an integrated, proactive component of the manufacturing process.
Core Principles and Regulatory Framework
The implementation of RTRT is guided by several core principles and an evolving regulatory landscape. From a technical perspective, RTRT relies on the establishment of valid combinations of measured material attributes and process controls that demonstrate maintained product quality [71]. This requires thorough process understanding and identification of Critical Process Parameters (CPPs) and Critical Quality Attributes (CQAs) that can be monitored in real-time [74].
Regulatory agencies worldwide have developed frameworks to support RTRT implementation. The FDA's Emerging Technology Program includes an Emerging Technology Team (ETT) that provides guidance for companies looking to employ RTRT [72]. Similarly, the European Medicines Agency (EMA) has established a "do and then tell" notification model that avoids processing stoppages while approvals are obtained [72]. These regulatory adaptations reflect a collaborative approach to modernizing quality assurance while maintaining rigorous safety standards.
The Integration of Artificial Intelligence in Pharmaceutical Quality Systems
AI Technologies Transforming Quality Assurance
Artificial Intelligence encompasses several technologies that are particularly transformative for pharmaceutical quality assurance. Machine Learning (ML), a fundamental paradigm of AI, uses algorithms that can recognize patterns within data sets [75]. A subfield of ML, Deep Learning (DL), engages artificial neural networks (ANNs) comprising interconnected sophisticated computing elements that mimic the transmission of electrical impulses in the human brain [75]. These include multilayer perceptron (MLP) networks, recurrent neural networks (RNNs), and convolutional neural networks (CNNs), which utilize either supervised or unsupervised training procedures [75].
In practical applications, these technologies enable powerful capabilities for quality systems. Natural Language Processing (NLP) can scan deviation reports to identify key details and automatically classify issues [76]. Predictive modeling with ML algorithms can detect statistical correlations across historical data to identify potential root causes of quality events [76]. These AI capabilities are being integrated into Quality Management Systems (QMS) to enhance deviation management, change control, and risk assessment processes [76].
AI Applications in Bioanalytical Method Validation
In the specific domain of bioanalytical validation, AI provides substantial advantages for method development, optimization, and troubleshooting. AI algorithms can accelerate method development by automating key steps such as optimizing chromatographic methods, performing peak deconvolution, and identifying patterns in complex data sets [76]. For instance, AI-driven tools can analyze historical chromatographic data to predict how a method will behave under new conditions, which is particularly valuable when working with expensive biologics [77].
Case studies demonstrate the tangible benefits of AI integration. In one implementation, a random forest model—a type of ML classification model—was trained on historical data from over 100 bioequivalence studies. When applied prospectively to 30 new formulations, it flagged high-risk candidates, reducing the need for approximately 40% of in vivo studies [77]. In another example, the WAND decision tree algorithm analyzed screening data from 150+ anti-idiotype antibody pairings and predicted the optimal reagent combination in under an hour, achieving a more than 70% reduction in development time while maintaining GLP-compliant documentation [77].
AI-Driven RTRT: Mechanisms and Implementation
Technical Architecture and Workflow Integration
The successful implementation of AI-enhanced RTRT requires a sophisticated technical architecture that integrates multiple systems and data flows. The workflow begins with data acquisition from Process Analytical Technology (PAT) tools, which represent the specific instruments used to quantify intermediate quality attributes (IQAs) [72]. Common PAT tools include Near-Infrared Spectroscopy (NIRS), which uses fiber optic probes and molecular vibrational motion to measure intermediate product quality [72]. These sensors gather real-time data that feeds into AI algorithms for continuous analysis and decision support.
The following diagram illustrates the integrated workflow of an AI-enhanced RTRT system:
This integrated approach enables continuous quality verification throughout manufacturing, allowing for immediate process adjustments when parameters trend toward specification limits [72] [73]. The AI system functions as a central decision support tool, analyzing patterns across multiple data streams to predict quality outcomes and recommend interventions.
The Research Toolkit for AI-Enhanced RTRT
Implementing AI-driven RTRT requires a specific set of technological components and analytical tools. The table below details essential research reagent solutions and their functions in establishing a robust RTRT system:
Table 1: Essential Research Toolkit for AI-Enhanced RTRT Implementation
| Tool/Technology | Function in RTRT System | Application Examples |
|---|---|---|
| Near-Infrared Spectroscopy (NIRS) | Non-destructive analysis of blend uniformity, moisture content, and potency | Monitoring powder blending, granulation endpoint detection [72] [74] |
| Machine Learning Algorithms (Random Forest, SVM) | Pattern recognition in multivariate process data, predictive modeling | Predicting dissolution based on material attributes, flagging high-risk candidates [75] [77] |
| Natural Language Processing (NLP) | Automated analysis of deviation reports and historical quality records | Root cause hypothesis generation, automated deviation classification [76] |
| Process Analytical Technology (PAT) Framework | System for designing, analyzing, and controlling manufacturing through timely measurements | Real-time monitoring of Critical Quality Attributes (CQAs) [72] [74] |
| Digital Validation Technologies (DVTs) | Integration with QMS, LIMS, and MES for streamlined validation | Automated documentation generation, enhanced data traceability [73] |
Comparative Analysis: Traditional Methods vs. AI-Enhanced RTRT
Performance and Efficiency Metrics
The transition from traditional quality control to AI-enhanced RTRT yields significant measurable benefits across multiple performance dimensions. The following table compares key metrics between these approaches:
Table 2: Performance Comparison: Traditional Quality Control vs. AI-Enhanced RTRT
| Performance Metric | Traditional Quality Control | AI-Enhanced RTRT | Data Source |
|---|---|---|---|
| Batch Release Time | Days to weeks post-manufacture | Potentially immediate after final manufacturing step | [72] [74] |
| Batch Failure Detection | End-process, after full batch completion | Intermediate stages, enabling material diversion | [72] |
| Sampling Frequency | Limited grab samples | High-frequency, continuous monitoring | [72] [74] |
| Investigation Time for Deviations | Manual, time-consuming root cause analysis | 50-70% reduction in investigation time | [76] |
| Process Flexibility | Limited, fixed parameters | High, with real-time parameter adjustments | [72] |
| Data Utilization | Limited to end-point testing | Comprehensive multivariate process data analysis | [75] [73] |
Case Studies in AI-Driven RTRT Implementation
Several pharmaceutical companies have pioneered the implementation of AI-enhanced RTRT with demonstrated success. AstraZeneca developed a system that blended PAT tools, in-process monitoring of parameters like tablet hardness, and cGMP practices at various stages of commercial tablet manufacturing. This approach obtained regulatory approval in Europe in 2007, representing one of the first implementations of its kind [72].
Eli Lilly contributed to the RTRT field through the development of a feed frame spectroscopic PAT tool that enabled real-time measurement of active ingredient concentration within the final blend of a pharmaceutical powder. After demonstrating its utility, this RTRT feed frame approach was adopted in several markets as part of the conventional control strategy [72].
In the domain of deviation management, AI implementation has demonstrated remarkable efficiency improvements. One case study describes an AI-driven process for investigating an out-of-specification (OoS) result for particulate matter in a sterile injectable product. The AI system automatically classified the deviation, retrieved similar historical events, and used ML models to identify the most likely root causes, reducing investigation time by 50-70% compared to conventional methods [76].
Methodological Protocols for AI-RTRT Integration
Experimental Framework for Method Validation
Integrating AI with RTRT within the ICH Q2(R1) validation framework requires a structured experimental approach. The protocol begins with Critical Quality Attribute (CQA) Identification, where AI algorithms analyze historical development and manufacturing data to identify parameters with the greatest impact on product quality [75] [76]. This is followed by Sensor Selection and Placement, determining appropriate PAT tools such as NIRS, and their optimal installation points within the manufacturing process to monitor identified CQAs [72] [74].
The core of the methodology involves Model Training and Validation, where ML algorithms are trained on extensive historical process data to establish correlations between process parameters, material attributes, and final product quality [75] [77]. This includes using techniques like cross-validation and back-testing to ensure model robustness. The final stage is Continuous Performance Monitoring, establishing systems to track model accuracy over time and trigger retraining when process or material changes occur [77] [76].
Protocol for AI-Assisted Root Cause Analysis
A specific experimental protocol for AI-assisted deviation investigation demonstrates the practical integration of AI into quality systems:
Deviation Intake and Automated Classification: Natural Language Processing (NLP) engines scan deviation reports to identify key details such as product, lot number, issue type, test method, and location [76].
Historical Pattern Analysis: ML models analyze historical deviation data to detect statistical correlations between similar events and potential contributing factors, ranking root causes by confidence level [76].
CAPA Recommendation Generation: AI systems propose structured corrective and preventive actions based on historical success rates, linking each proposed CAPA to relevant SOPs, equipment, and documentation [76].
Implementation Tracking: Live dashboards update automatically with risk scores, due dates, and progress metrics, enabling continuous monitoring of CAPA effectiveness [76].
Challenges and Future Directions
Implementation Challenges
Despite its significant benefits, the adoption of AI-enhanced RTRT faces several substantial challenges. The regulatory landscape for RTRT is more complex than traditional analytical testing and continues to evolve as these methods integrate into industry standards [72]. Global harmonization remains challenging, with different regulatory bodies implementing varying digital strategies and acceptance criteria [72] [77].
From a technical perspective, implementation represents a major challenge requiring a high level of process understanding and an acceptable risk/cost ratio [72]. Practical requirements such as developing reference methods to validate sensors can demand significant time and financial investment [72]. Additionally, the quantity of data generated increases exponentially due to high-frequency sampling, creating intensified needs for data storage, traceability systems, and specialized personnel [72].
Cultural and organizational barriers also present significant hurdles. Implementation requires large-scale capability shifts and increases in employees specializing in PAT and data science [72] [71]. Furthermore, maintaining and updating PAT tools and sensor equipment demands specialized expertise that may not exist within traditional pharmaceutical quality organizations [72].
Emerging Solutions and Future Trends
The pharmaceutical industry is developing innovative solutions to address these challenges. To enhance regulatory acceptance, approaches such as "explainable AI" techniques including LIME (Local Interpretable Model-agnostic Explanations) are being implemented to provide step-by-step rationales for AI decisions [77]. Maintaining "humans-in-the-loop" at critical checkpoints ensures that AI recommends while humans decide, with thorough documentation of both components [77].
From a technological perspective, continued advances in on-line and in-line sensor technologies are crucial for the biopharmaceutical manufacturing industry to achieve the full potential of RTRT [71]. Integration with Digital Validation Technologies (DVTs) creates a unified validation ecosystem that connects Quality Management Systems (QMS), Laboratory Information Management Systems (LIMS), and Manufacturing Execution Systems (MES) [73].
The future direction points toward increasingly autonomous systems, as exemplified by developments in Validation 4.0, which leverages AI and digital technologies to enable continuous visibility and proactive decision-making [73]. This represents a fundamental shift from static validation approaches to dynamic, data-driven strategies that ensure processes remain in a validated state through continuous monitoring [73].
The integration of Artificial Intelligence with Real-Time Release Testing represents a transformative advancement in pharmaceutical quality assurance. This synergy moves the industry from traditional document-heavy, retrospective quality control toward dynamic, data-driven approaches that offer increased efficiency, enhanced product quality, and reduced time-to-market. AI-enhanced RTRT enables a fundamental shift from detecting quality issues after they occur to predicting and preventing them through continuous process monitoring and intelligent analysis.
The successful implementation of this paradigm requires addressing significant challenges related to regulatory alignment, technical infrastructure, and organizational capability. However, case studies from industry leaders demonstrate that these hurdles can be overcome with substantial benefits. As the industry progresses toward Validation 4.0, the combination of AI and RTRT positions pharmaceutical companies to meet evolving regulatory expectations while accelerating patient access to critical medicines. For researchers and drug development professionals, mastering these technologies is becoming essential for advancing pharmaceutical manufacturing in the 21st century.
Conclusion
Successfully validating analytical methods for pharmaceutical residue analysis according to ICH Q2(R1) is fundamental to ensuring patient safety and regulatory compliance. This guide has synthesized the journey from understanding core principles to implementing practical, robust procedures and managing their entire lifecycle. The key takeaway is that a science- and risk-based approach, as championed by modern guidelines, leads to more reliable and adaptable methods. Looking forward, the integration of QbD principles, the adoption of advanced technologies like AI and real-time monitoring, and the ongoing harmonization of global standards will continue to enhance the efficiency, accuracy, and overall quality of pharmaceutical analysis, ultimately accelerating the delivery of safe and effective medicines to patients.
References
- 1. Analytical Strategies for Monitoring Residual Impurities ... [https://www.bioprocessintl.com/process-monitoring-and-controls/analytical-strategies-for-monitoring-residual-impurities-encountered-in-bioprocessing]
- 2. Analytical Strategies for Monitoring Residual Impurities [https://www.biopharminternational.com/view/analytical-strategies-monitoring-residual-impurities]
- 3. Process Related Impurities and Residuals Analysis [https://www.intertek.com/pharmaceutical/biopharmaceuticals/process-residuals/]
- 4. ICH Q2(R1) Validation of Analytical Procedures [https://www.gmp-compliance.org/guidelines/gmp-guideline/ich-q2r1-validation-of-analytical-procedures-text-and-methodology]
- 5. ICH and FDA Guidelines for Analytical Method Validation [https://www.labmanager.com/ich-and-fda-guidelines-for-analytical-method-validation-34252]
- 6. ICH Guidance; Validation of Analytical Procedures: Text ... [https://jordilabs.com/lab-testing/regulatory/ich-q2-r1/]
- 7. Method categories according to the ICH Q2(R1) - Lösungsfabrik [https://mpl.loesungsfabrik.de/en/english-blog/method-validation/method-categories]
- 8. Q2(R1) Validation of Analytical Procedures: Text and ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/q2r1-validation-analytical-procedures-text-and-methodology-guidance-industry]
- 9. A Review: Comparison of ICH Guidelines on Analytical ... [https://www.linkedin.com/pulse/review-comparison-ich-guidelines-analytical-method-usp-shaikh-wzfjc]
- 10. Highlights from FDA's Analytical Test Method Validation ... [https://www.propharmagroup.com/thought-leadership/fda-analytical-test-method-validation-guidance]
- 11. Navigating the Biopharmaceutical Method Validation [https://synergbiopharma.com/navigating-the-evolution-from-ich-q2r1-to-ich-q2r2-and-implementation-of-ich-q14-in-biopharmaceutical-method-validation/]
- 12. Quo Vadis Analytical Procedure Development and ... [https://www.chromatographyonline.com/view/quo-vadis-analytical-procedure-development-and-validation-]
- 13. Key ICH Method Validation Parameters to Know [https://altabrisagroup.com/ich-method-validation-parameters/]
- 14. Limit of Blank, Limit of Detection and Limit of Quantitation [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556583/]
- 15. Comparison of approaches for assessing detection and ... [https://www.nature.com/articles/s41598-024-83474-5]
- 16. Comparison of Different Approaches for Calculating LOD ... [https://ps.tbzmed.ac.ir/Article/ps-40452]
- 17. Determining LOD and LOQ Based on the Calibration Curve [https://www.sepscience.com/hplc-solutions-126-chromatographic-measurements-part-5-determining-lod-and-loq-based-on-the-calibration-curve-6959]
- 18. Limit of Quantitation - an overview [https://www.sciencedirect.com/topics/nursing-and-health-professions/limit-of-quantitation]
- 19. Method Validation Essentials, Limit of Blank ... [https://www.biopharminternational.com/view/method-validation-essentials-limit-blank-limit-detection-and-limit-quantitation]
- 20. A tutorial for computing limits of detection and ... [https://www.sciencedirect.com/science/article/abs/pii/S0003267021011685]
- 21. Current Good Manufacturing Practice (CGMP) Regulations [https://www.fda.gov/drugs/pharmaceutical-quality-resources/current-good-manufacturing-practice-cgmp-regulations]
- 22. Good manufacturing practice | European Medicines Agency ... [https://www.ema.europa.eu/en/human-regulatory-overview/research-development/compliance-research-development/good-manufacturing-practice]
- 23. Drug Compliance Programs [https://www.fda.gov/drugs/guidance-compliance-regulatory-information/drug-compliance-programs]
- 24. FDA Issues New Guidance on Current Good Manufacturing ... [https://www.arnoldporter.com/en/perspectives/advisories/2025/01/fda-guidance-good-manufacturing-practices-for-drugs]
- 25. New EU Guidelines Simplify Medicines Lifecycle ... [https://gmdpacademy.org/news/streamlining-change-new-eu-guidelines-simplify-medicines-lifecycle-management/]
- 26. ICH Guidelines for Analytical Method Validation Explained [https://amsbiopharma.com/ich-guidelines-analytical-method/]
- 27. Key Validation Characteristics in ICH Q2 [https://altabrisagroup.com/validation-characteristics-ich-q2/]
- 28. Forced degradation studies: A critical lens into ... [https://www.clinicaltrialsarena.com/sponsored/forced-degradation-studies-a-critical-lens-into-pharmaceutical-stability/]
- 29. Forced Degradation Studies: Regulatory Considerations ... [https://www.biopharminternational.com/view/forced-degradation-studies-regulatory-considerations-and-implementation]
- 30. Forced Degradation Studies for Stability [https://www.nelsonlabs.com/testing/forced-degradation/]
- 31. Forced Degradation Studies | ICH Stability Testing [https://biopharmaspec.com/protein-characterization-services/forced-degradation-studies/]
- 32. Peak Purity in Liquid Chromatography, Part I [https://www.chromatographyonline.com/view/peak-purity-liquid-chromatography-part-i-basic-concepts-commercial-software-and-limitations]
- 33. A Standardized 2D-LC Screening Platform for Peak Purity ... [https://www.chromatographyonline.com/view/a-standardized-2d-lc-screening-platform-for-peak-purity-determination-in-pharmaceutical-analysis]
- 34. A strategy for assessing peak purity of pharmaceutical ... [https://www.sciencedirect.com/science/article/abs/pii/S0021967323001024]
- 35. Evaluation of Swab and Rinse Sampling Procedures ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7758009/]
- 36. Accuracy and Precision - What's The Difference? [https://scioninstruments.com/us/blog/accuracy-and-precision-whats-the-difference/]
- 37. What is the ICH Q2(R2) guideline? - Lösungsfabrik [https://mpl.loesungsfabrik.de/en/english-blog/method-validation/ich-q2r1]
- 38. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 39. Study and ICH validation of a reverse-phase liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5762446/]
- 40. Cleaning Validation: Regulatory Expectations and ... [https://contractlaboratory.com/cleaning-validation-regulatory-expectations-and-methodologies/]
- 41. Cleaning validation in pharmaceutical quality control ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12229404/]
- 42. Mastering APIC Cleaning Validation [https://www.leucine.io/cleaning-validation-blogs/apic-cleaning-validation]
- 43. Cleaning Validation Program Maintenance in a Process ... [https://ispe.org/pharmaceutical-engineering/january-february-2021/cleaning-validation-program-maintenance-process]
- 44. Determination of Cleaning Limits Considering ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8170751/]
- 45. Analytical Methods for Cleaning Validation [https://pharmallies.com/choosing-the-right-analytical-methods-for-cleaning-validation/]
- 46. ICH Q2(R2) Validation of Analytical Procedures [https://www.qbdgroup.com/en/blog/ich-q2r2-validation-of-analytical-procedures-an-overview-of-the-revised-guideline/]
- 47. Best Practices for Cleaning Validation Swab Recovery ... [https://www.pharmtech.com/view/best-practices-cleaning-validation-swab-recovery-studies]
- 48. 9 Proven Ways to Avoid Failing Methods Due to Low Limits [https://www.leucine.io/cleaning-validation-blogs/9-proven-ways-to-avoid-failing-methods-due-to-low-limits]
- 49. Your Comprehensive Guide to Swab Cleaning Validation [https://blog.puritanmedproducts.com/your-comprehensive-guide-to-swab-cleaning-validation]
- 50. Swab vs Rinse Sampling: Methods and Applications [https://www.linkedin.com/posts/mahesh-kushwah-525aa522a_q36-what-is-the-difference-between-swab-activity-7373671615085268992-pwEc]
- 51. Comparing Swab and Rinse Results [https://cleaningvalidation.com/memos/comparing-swab-and-rinse-results/]
- 52. Validation of Cleaning Residue Analysis (Swab & Rinse ... [https://www.webofpharma.com/2025/11/ensuring-manufacturing-cleanliness.html]
- 53. a structured protocol for contamination risk mitigation [https://link.springer.com/article/10.1007/s40199-025-00566-x]
- 54. Carbon Measurement Methods for Cleaning Validation [https://www.pharmtech.com/view/carbon-measurement-methods-cleaning-validation-comparing-direct-combustion-rinse-and-swab-sampling-m]
- 55. Guidance Summary | Rinsate and Swab Sample [https://www.gmpsop.com/site-overview/guidance-summary/guidance-summary-11-20/]
- 56. Best Practices For Successful Method Validation [https://lgmpharma.com/blog/best-practices-for-successful-method-validation/]
- 57. Where Do Interference Peaks in Liquid Chromatography ... [https://universallab.org/blog/where_do_interference_peaks_in_liquid_chromatography_come_from]
- 58. Integration Errors in Chromatographic Analysis, Part I [https://www.chromatographyonline.com/view/integration-errors-chromatographic-analysis-part-i-peaks-approximately-equal-size]
- 59. Real Solutions to Improve Your HPLC Peak Resolution [https://www.thermofisher.com/blog/analyteguru/real-solutions-to-improve-your-hplc-peak-resolution/]
- 60. Understanding ICH ( Q ): 2 of R Procedures in the... 1 Validation Analytical [https://iampharmacist.com/2025/05/31/ich-q2r1/]
- 61. Determination of Pharmaceutical Residues by UPLC-MS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7811430/]
- 62. Analytical Quality by Design and Analytical Procedure Life Cycle [https://qualitymatters.usp.org/paradigm-shift-drug-development-analytical-quality-design-and-analytical-procedure-life-cycle]
- 63. AQbD-novel strategy for analytical methods [https://fjps.springeropen.com/articles/10.1186/s43094-024-00706-1]
- 64. Aspects and Implementation of Pharmaceutical Quality by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12114689/]
- 65. Analytical Method Validation for Quality Assurance and ... [https://www.americanpharmaceuticalreview.com/Featured-Articles/569734-Analytical-Method-Validation-for-Quality-Assurance-and-Process-Validation-Professionals/]
- 66. Pharmaceutical Cleaning Validation - Residue Detection ... [https://technotes.alconox.com/industry/medical-device/pharmaceutical-cleaning-validation-residue-detection-method-selection/]
- 67. Methods for Detecting Residues of Cleaning Agents During ... [https://journal.pda.org/content/54/5/365]
- 68. What are the differences and key steps in Analytical ... [https://resources.eirgenix.com/blog/method_dev_qual_validation]
- 69. Qualification Vs Validation: Understand The Key Differences [https://gmpinsiders.com/qualification-vs-validation-key-differences/]
- 70. Risk-Based Continued Test-Method Performance ... [https://ispe.org/pharmaceutical-engineering/january-february-2022/risk-based-continued-test-method-performance]
- 71. Opportunities and challenges of real-time release testing in ... [https://pubmed.ncbi.nlm.nih.gov/28710854/]
- 72. Real-Time Release Testing in Pharmaceutical Manufacturing [https://www.news-medical.net/life-sciences/Real-Time-Release-Testing-in-Pharmaceutical-Manufacturing.aspx]
- 73. The Transformative Impact of Artificial Intelligence on ... [https://perfval.com/artificial-intelligence-in-validation/]
- 74. Real Time Release Testing [https://www.pharmtech.com/view/real-time-release-testing]
- 75. Artificial intelligence in drug discovery and development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7577280/]
- 76. Artificial Intelligence in Biopharmaceutical Quality ... [https://www.bioprocessintl.com/information-technology/a-vision-for-artificial-intelligence-in-biopharmaceutical-quality-management-systems]
- 77. How AI is Reshaping Compliance with Smart Bioanalytical ... [https://www.bioanalysis-zone.com/how-ai-is-reshaping-compliance-with-smart-bioanalytical-validation/]